Summary
- “By connecting to what matters to our patients, we are reconnecting to what matters to our own hearts as health care professionals.”
In my role as Director of Continuing Professional Development & Clinical Implementation at Sutter Health, I am amazed by the paradigm-shifting approaches to patient care that I see every day. Our Roseville Medical Center facility in California has been piloting an Awake and Walking model of critical care for a couple of years now. With this approach, the team works to care for patients while keeping them conscious (as opposed to medically sedated), aware, and mobile. This type of critical care lets patients connect to what matters most to them — whatever it is that’s feeding their will to live. It reduces medications that can cause harm, such as continuous sedation. Continuously sedated patients are often restrained, which impedes mobility and is a risk factor for post-traumatic stress disorder (PTSD). By helping patients mobilize, the model also reduces the risk of delirium and dementia. All of these pieces combine to support age-friendly care for older adults.
Joining the Movement
I've been a member of the American Delirium Society for a very long time and deeply involved in their leadership, trying to find strategies to address the same entrenched gaps between evidence and practice. I learned about the Age-Friendly Health Systems movement through Christine Waszynski, DNP, APRN, GNP-BC, FAAN, a mentor and friend, and a powerful presentation by Terry Fulmer, PhD, RN, FAAN, President of The John A. Hartford Foundation, who ignited the movement.
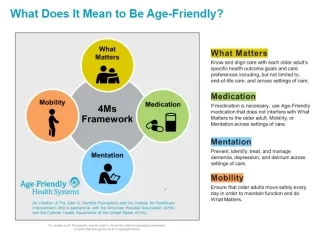
Figure 1. 4Ms Framework of an Age-Friendly Health System
The 4Ms Framework of Age-Friendly Care (What Matters, Medication, Mentation, Mobility) had a lot of appeal. It hits on so many of the key components that we care about for all ages. Later, I joined with the two of them and others to coauthor an article describing the potential for the 4Ms to optimize delirium care.
Due to the evidence base of the movement and alignment with Sutter Health’s mission, when I pitched becoming an Age-Friendly Health System to the C-suite, the response was, “You had us at hello.” It’s a worthwhile endeavor for our health system to be a leader in this work.
Increasing Joy and Reducing Burnout
One of the biggest risk factors for burnout in health care is when we start to practice in a way that is misaligned with our core values or our ethics.
At an early age, I got a job working on an ambulance. I loved it. I had this idea that it was all about saving lives. I had a couple of experiences that made me realize that it’s also about being a healing presence, even (or especially) in situations where there is no possible health care intervention.
I have heard now from physical therapists, from nurses and physicians, that the process of implementing age-friendly care is making them feel more joy in their work. They feel less burned out, more connected to their values. That’s huge. By connecting to what matters to our patients, we are reconnecting to what matters to our own hearts as health care professionals.
Career Impact
While I've been engaged in delirium, brain health, and mentation as a whole for more than a decade, I’ve had the opportunity to learn more about the other “Ms” in the 4Ms framework to help our team find new assessment tools and support updated protocols.
My work in education has always included identifying and addressing practice gaps through interprofessional collaboration. Now, I’m looking at gaps at the system and community level through cross-sector community partnerships. The focus is on what we can do to build age-inclusive community resilience at a time when a lot of vulnerable individuals are having their safety net taken away. This work has also led to publishing opportunities. As a nurse, I never would have imagined that I’d have an upcoming article in a community planning journal.
Be recognized as a leader in age-friendly care. Prepare for the Certified Professional in Age-Friendly Health Care credential
Florence’s Care
Florence* had just recently been extubated when I met her and her daughter. She was in critical care on a ventilator in a different state. As soon as she was well enough to be discharged, her family brought her to California. Unfortunately, she had a lot of complications and she needed to be rehospitalized, this time at Roseville. The team managed her entire time on the ventilator under the Awake and Walking model.
Florence said she believed in her heart of hearts that the only reason she was still alive was because of how her care was managed at Roseville — using an age-friendly approach. She was alert, connected to her family, and able to do what mattered most to her, which was to pray every day with her family. She was given autonomy to make decisions about her care, such as whether to begin continuous dialysis.
Florence’s daughter said she felt like there was a partnership between the health care team, her, and her mom. She felt less anxiety because her mom could speak for herself and make her own decisions. They also believed the ability to connect with family every day was an element of her healing.
It was so powerful for me as a health care professional to hear how Florence felt about her level of care. Here’s a person who unfortunately had two encounters with critical care, and she felt that the care we provided saved her life.
Working Together
There’s not a single person who’s not aging. We all care deeply about somebody who is already an older adult. I got involved in delirium after being a family caregiver for my dad for more than a decade. He had a very severe episode of delirium that was never addressed when he was in acute care.
In many instances, health care has fallen short in meeting the needs of our loved ones or ourselves. We can make significant improvements if we all agree, collectively, that we’re going to work on it together.
*Not the patient’s real name.
Kerri Maya, PhD(c), MSL, RN, NPD-BC, is Director of Continuing Professional Development & Clinical Implementation at Sutter Health.
Photo by Jamie Street on Unsplash
You may also be interested in:
Join the Age-Friendly Health Systems movement
Kerri Maya and other experts reflect on a tool for engaging older adults and caregivers on the 4Ms (scroll down to watch videos)
