Aging with Intention: How the 4Ms and My Health Checklist Can Guide Care for Veterans and Their Families
Summary
- As our Veteran community ages, the question before us is not just how long we can live, but how well we can live.
What do Veterans, caregivers, and service members most want to see prioritized in health care systems? The results of a survey at the MCON Health Summit 2025 are revealing: 63 percent of Veterans and military families surveyed said they want resources focused on caring for aging Veterans, ranking it as the second-highest priority, right after improving military culture training for civilian health care providers.
Our military-connected community is ready to talk about aging, longevity, and the kind of care that sustains quality of life. At the nonprofit organization PsychArmor, we are answering that call by building education, partnerships, and practical tools that honor the entire continuum of military and Veteran life.
Why Aging Conversations Matter in the Military-Connected Community
Military experiences, deployments, and transitions shape how Veterans age, how they view independence, and how they engage with health systems. Yet many health care providers remain unprepared to address these complex realities. Conditions such as post-traumatic stress disorder (PTSD), traumatic brain injury (TBI), chronic pain, moral injury, and social isolation all interact with aging in unique ways.
That’s why the 4Ms Framework of an Age-Friendly Health System, an initiative of The John A. Hartford Foundation and IHI, and tools like My Health Checklist are so valuable. They serve as roadmaps for care, helping Veterans articulate their goals, preferences, and priorities before, during, and after medical appointments.
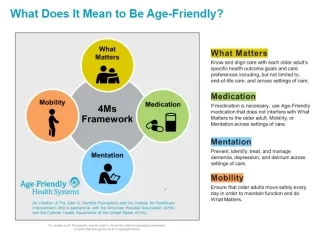
The 4Ms in Practice: A Veteran Lens
1. What Matters
For many Veterans, “what matters” extends beyond medical goals. It’s about legacy, belonging, and purpose. It might mean staying in their home, remaining connected to battle buddies, or ensuring their care through the end of life reflects their values and beliefs.
Veterans and caregivers can use My Health Checklist to record these goals and values.
Providers can ask:
• “How has your service shaped what matters most to you today?”
• “Are your health plans and end-of-life wishes clearly documented and honored?”
2. Medication
Many Veterans receive prescriptions from both the Department of Veterans Affairs (VA) and community providers. Without coordination, this can lead to duplication, side effects, and confusion.
Veterans can list all medications — VA, non-VA, and over-the-counter medications — in their My Health Checklist.
Providers can use this information to align treatments with the Veteran’s priorities and to uphold what matters most to them.
3. Mind (Mentation)
Cognitive health must be understood through the lens of trauma, memory, and meaning. Veterans may experience dementia layered with PTSD, depression, or grief. Through the 4Ms, mind/mentation becomes not just a clinical checkpoint, but a commitment to trauma-informed, culturally competent care.
Veterans and caregivers can document mood changes, memory concerns, or triggers in their checklist.
Providers can screen compassionately and connect Veterans with mental health and caregiver support.
4. Mobility
Military service often leaves lasting physical impacts that affect mobility with age. Encouraging safe daily movement preserves function and confidence, whether through adaptive exercise, therapy, or simply engaging with community life.
Providers can assess gait and fall risk while ensuring mobility goals reflect what matters, being present for milestones, engaging in hobbies, and maintaining dignity in motion.
Partnership in Action
This year, PsychArmor proudly began partnering with the San Diego State University Center for Excellence in Aging & Longevity (CEAL) to explore how aging and caregiving intersect within military-connected families. This partnership bridges research, education, and lived experience, ensuring that future programs reflect the real challenges and hopes of those navigating care transitions.
Together, we are developing resources to support Veterans, their caregivers, and care teams. Our shared goal: to make every care environment, from hospital to home, both age-friendly and Veteran-ready.
Bringing It All Together: My Health Checklist for Veterans
My Health Checklist is more than a form; it is a conversation starter. It can help Veterans prepare for medical appointments, identify priorities, list medications, and document what truly matters. Providers can use it as a tool to listen deeply, document clearly, and act on what they hear. When paired with 4Ms care, the checklist becomes a bridge between the health care system and the Veterans' health priorities, while helping everyone on the care team align around a shared purpose.
Aging as the Next Mission
The data from MCON 2025 is clear: aging and longevity must become a national priority for the military and Veteran community. PsychArmor is committed to leading that charge, through education, partnership with organizations such as The Conversation Project, and dialogue that honors Veterans across the entire life continuum. Talking about aging, caregiving, and end-of-life is not always easy, but it is essential. The more we share our stories, the more we build systems that see the person behind the patient.
Looking ahead, PsychArmor and The Conversation Project are joining forces in 2026 to deepen the national dialogue around aging, caregiving, and end-of-life readiness within the military-connected community. Stay tuned!
Dr. Qwynn Galloway-Salazar is the SVP of Engagement & Transformation at PsychArmor.
Photo by Kateryna Hliznitsova on Unsplash
You might also be interested in:
- VA Age-Friendly Health Systems Initiative
- 5 Actions to Take Across November to Support your Personal, Social, or Community Circles
- Centering What Matters: The Core of Age-Friendly Care
