Why It Matters

Grady Health is a public academic health care system that is serious about its mission to care for the residents of metro Atlanta, Georgia. Its flagship facility, Grady Memorial Hospital, is a safety net hospital that serves all patients regardless of their insurance status or ability to pay. For their care providers — including their physicians, who serve on the faculties of the Emory School of Medicine and the Morehouse School of Medicine — equity and cultural competence are key to providing high-quality care.
Caring for the residents of metro Atlanta means serving a rapidly aging population. Data indicates that 10 percent of metro Atlanta is over the age of 60 and that percentage is predicted to double by 2030. At Grady, patients aged 65 and older account for 38 percent of hospital admissions and 49 percent of hospital days.
Consequently, Grady has been working for years to improve care for older adults. It received its designation as a NICHE (Nurses Improving Care for Healthsystem Elders) hospital in 2014. It subsequently established an acute care for elders (ACE) unit, spearheaded by Ugochi Ohuabunwa, MD, Emory’s Chief of Geriatrics at Grady Memorial.
In 2020, Grady joined Age-Friendly Health Systems (AFHS), an initiative of the Institute for Healthcare Improvement (IHI) and The John A. Hartford Foundation in partnership with the American Hospital Association and the Catholic Healthcare Association of the US. Through AFHS, said Vonetta Daniels, Director of Care Logistics at Grady and AFHS Project Manager, “We’re building on the success of the ACE unit" and other age-friendly care processes implemented within the health care system.
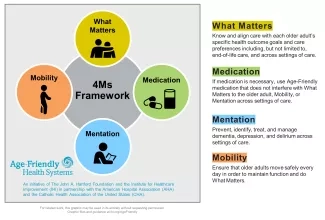
Joining AFHS means committing to age-friendly care, defined as evidence-based care that includes the 4Ms — What Matters, Medication, Mentation, and Mobility (Figure 1) — causes no harm, and is grounded in What Matters to the older adult.
Grady decided to add an additional M to the 4Ms framework — Malnutrition — because staff knew that 25-30 percent of their hospitalized older adults were malnourished. Many of their patients, said Daniels, are “deciding between filling their prescriptions and buying groceries.”
Since food insecurity and poor nutrition carry greater risks with age, they are piloting the 4Ms + Malnutrition work on the ACE unit, using Plan-Do-Study-Act (PDSA) cycles. “It’s the first draft of workflow,” said Daniels. “We want to get it crystallized,” and then roll it out to other units. Their team includes a project sponsor (Ohuabunwa), project manager (Daniels), and a lead for each of the 4Ms + Malnutrition. Nursing informatics and nursing education are also essential to this team effort.
The following overview describes some of the ways they are implementing each of the 4Ms + Malnutrition:
What Matters — The team established a What Matters Advisory Group composed of six older adults who helped developed the questions to be asked to determine patients’ goals. Their guidance includes:
Be at the patient's level. If the patient is in bed, don’t stand. Sit next to the patient so you’re at eye level.
After asking a question, listen. Don’t start writing until you’re sure you understand the answer.
Based on input from the Advisory Group, the team incorporated new questions into the electronic health record (EHR) to ask all older adults at admission:
What concerns you most when you think about your health?
What would be a good outcome from your visit?
What things are important to you in your life?
What brings you joy?
In addition to these intake questions, the team also asks older adults two questions every day:
What are your goals for today?
How can we help you to achieve them?
The team uses these questions to develop an overall goal for the day, mobility goals, and cognitive activity goals with patients. They write these goals on white boards so the entire care team will be aware of them.
Medication — Grady’s pharmacy team worked with the EHR team to create an alert that warns against prescribing medications on the Beers Criteria Medication List, which indicates potentially inappropriate medications for older adults. The alert also links to safer substitutes. “You don’t want to put that alert in without offering alternatives,” said Daniels. While the physician can still use discretion, Daniels says that this system is user-friendly and offers helpful guidance to minimize prescribing inappropriate medications. In addition, Grady uses the ACE Tracker, a checklist that pulls information from multiple areas of the EHR to identify risk factors for functional decline and poor outcomes among older adults. The ACE tracker also flags high-risk medicines, and the clinical staff can provide feedback to the patients’ providers and offer safer alternatives.
Mentation — The team uses the Nursing Delirium Screening Scale (Nu-DESC), the Patient Health Questionnaire (PHQ) for depression and anxiety, and the Six-Item Screener for cognitive impairment. They also use the AWOL assessment to predict the risk of delirium during hospitalization. They subsequently screen for delirium every 12 hours using the Nu-DESC tool and then incorporate these assessments into hourly rounding and the bedside shift report.
To help prevent delirium from developing, the team asks patients about activities they enjoy and offers activity bags that correspond to their interests. Examples include music, reading, puzzles, chess, or crocheting. These activities are then incorporated into patients’ daily routines with the help of volunteers (pre-pandemic), patient safety monitors, or nurses.
Mobility — Across the hospital, Grady is prioritizing a mobility program called Get Up and Go that was developed by their physical therapists. The program encourages nurses to do an early evaluation of patient mobility. Nurses mobilize patients based on their mobility scores, engage them in planned activities, and use a device that assists with getting patients out of bed. They incorporate mobility recommendations into rounds and bedside shift reports, with a mobility plan developed by the patients and nurses during the bedside shift change.
Malnutrition — Nurses at Grady use a two-pronged approach to address nutrition. They screen older adults for malnutrition at intake. Signs they look for include weight loss, loss of muscle mass, and diminished hand grip strength. They follow the ASPEN guidelines. A dietician then does an assessment for malnutrition risk and food insecurity. During hospitalization, mealtime rounds are conducted daily, monitoring patients’ food intake, and providing assistance and meal supplements as needed. Prior to discharge, the team again assesses nutrition needs and food security. When appropriate, older adults are referred to an organization called Open Hand for 10 free meals after discharge.
One of the key aspects of integrating the 4Ms + Malnutrition into care is ensuring that information is recorded and shared. “That bedside shift report is a critical piece,” said Ohuabunwa, helping the team to create a plan for the day to address all the Ms. White boards are also key, providing a place for care team members to see and record the older adult’s goals for the day, and information about the 4Ms + Malnutrition. They also document this information in the EHR.
Next Steps
Some data indicates reductions in length of stay for patients 65 and older on some units since implementing the 4Ms. Grady plans to introduce other metrics to assess progress, including injury from falls, pressure ulcers, hospital-acquired infections, adverse medication events, and readmissions.
Grady is currently seeking grant funding for a proposed pilot project to give tablets to all older patients during their hospital stay that they could take home to keep. With tablets, older adults could communicate with friends and family, listen to free AARP concerts, and engage in other activities to help address What Matters and Mentation. Giving patients these devices could also help them connect with telehealth and community resources (see below) after discharge. Their plan includes teaching or reinforcing digital literacy skills during hospitalization.
The team is also fostering community partnerships to create a stronger continuum of care for older adults. Their partners include United Way of Greater Atlanta, AARP Georgia, Open Hand, and Jesse Hill Market.
The Grady team reports that the AFHS framework and working with IHI has helped to get leadership support, which has been invaluable to their progress. “This is a framework by IHI; it’s not just me saying, ‘I would like to disseminate this,’” explained Ohuabunwa. “The fact that we have the framework, the backing of IHI, and the action community [of fellow AFHS participants] has helped us with the implementation.”
You may also be interested in:
