Why It Matters
A physician couldn't believe it when she calculated that improving delirium care led to a massive return on investment. She then learned that her cost and length of stay estimates were conservative.
We know that age-friendly care is good for older adults, but demonstrating cost savings can be challenging. For the University of Texas Health Science Center at Houston (UT Health), making the effort to crunch the numbers has been worth it. The return on investment (ROI) they’ve uncovered has been astonishing.
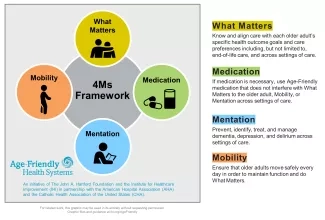
UT Health’s Min Ji Kwak, MD, MS, DrPH, has used the ROI calculator developed by the Institute for Healthcare Improvement (IHI) to assess the financial impact of age-friendly care in her health system (see The Business Case for Becoming an Age-Friendly Health System). Kwak is an assistant professor at UT Health who also works at UT Health’s teaching hospital, Memorial Hermann-Texas Medical Center. UT Health participates in Age-Friendly Health Systems (AFHS), an initiative of IHI and The John A. Hartford Foundation in partnership with the American Hospital Association and the Catholic Healthcare Association of the US. AFHS defines age-friendly care as evidence-based care that includes the 4Ms — What Matters, Medication, Mentation, and Mobility — causes no harm, and is grounded in What Matters to the older adult (see Figure 1 below).
Assessing the Impact on Delirium
Approximately 140-150 older adults are admitted to Memorial Hermann’s cardiac intensive care unit (CCU) and cardiac intermediate care unit (CIMU) every month. Older adults in the CCU and the CIMU tend to be particularly vulnerable to delirium, so Kwak and her team chose to start implementing the 4Ms there. They started planning in August 2019 and began implementation in September 2019.
As they started screening for delirium, the rate increased from about 6 percent to about 11 percent. They attributed this to increased screening identifying more cases. As they started implementing the 4Ms, the rate began to fall. Specifically, they implemented both Medication and Mentation activities that likely helped to prevent delirium. A pharmacist reviewed the medication list for every patient, and the electronic health record included an alert for potentially inappropriate medication for older adults. The team also provided older adults with reading glasses and hearing amplifiers to help them remain alert, as well as puzzles and games to mentally engage them. By December 2019, the rate of delirium fell to 5 percent.
Typical responses to delirium include prescribing medications such as haloperidol and lorazepam, using restraints, and having a sitter stay with the patient. From April to October 2019, all these orders declined, most by a significant percentage. For instance, the use of sitters declined from 4.11 percent to 2.55 percent. This is particularly relevant for the business case because insurers, including the Centers for Medicare and Medicaid Services (CMS), don’t usually reimburse hospitals for the cost of using sitters.
Using the ROI Calculator
After seeing these improvements, Kwak used the ROI calculator to estimate the overall cost of implementing the 4Ms. She entered her estimate of the number of annual admissions (2,000), then input expenses, including walkers, canes, hearing amplifiers, reading glasses, and the geriatrician’s time. The total came to $46,000.
To calculate savings, Kwak focused on delirium and length of stay (LOS) because delirium can contribute to longer LOS. Kwak calculated the initial incidence of delirium, and then the percentage reduction in the incidence attributed to the program. Going from about 11 percent to about 5 percent meant there was a 54.5 percent reduction in delirium. (Kwak noted that she almost thought there was a 6 percent reduction because “11-5 = 6” is more intuitive. She cautions others to be careful when doing these types of calculations.)
In her hospital, the average LOS in the units was five days, and the average cost per day was $2,010. Kwak speculated that delirium would increase the LOS by two days and would require extra sitter use during those two days. She estimated that the daily cost for sitters was $260. The total added hospital case cost, therefore, would be $4,540.
After taking reimbursement into account, the calculator determined that the program had avoided $693,622 in costs. Subtracting the estimated cost of $46,000, the net benefit was estimated to be $647,622. The ROI was 1407.9 percent.
“This number was shockingly high,” said Kwak. She ran the numbers by a member of the hospital’s operations team and learned that her estimates for cost and length of stay were conservative. Therefore, Kwak said, “I strongly believe that the 4Ms initiative return is significantly high.”
She added, “Based on my experience, the ROI calculator is very user-friendly.” It gives detailed instructions, and the summary is concise and easy to understand.
Spreading the 4Ms
Kwak and her team initially planned to present this work to the executive leadership of the hospital, thinking that a top-down approach might expedite the spread of the initiative. But then the pandemic complicated matters, and they have not yet had the opportunity to make that presentation.
Instead, said Kwak, “I took a different route — a bottom-to-top approach.” She started presenting data to different units in the hospital, and it quickly caught their attention. Now, other acute cardiac units, including intensive cardiac units specializing in cardiovascular surgery or heart failure patients, are participating in the initiative. As next steps, Kwak and her team are engaging the hospitalist group and trauma units.
“It is still a work in progress,” she said, “but I hope that one day, our initiatives will be the standard for our hospital. And I believe that we are getting there.”
You may also be interested in:
Resources to Practice Age-Friendly Care, including The Business Case for Becoming an Age-Friendly Health System
Spread Is No Accident: Linking Age-Friendly Improvement to Strategic Priorities
