Why It Matters
Hartford HealthCare saw a 43 percent reduction in falls and a 40 percent overall reduction in delirium-attributable days after implementing the Age-Friendly 4Ms.
When it comes to health care interventions, spread doesn’t happen automatically; tested strategies are needed to spread these interventions throughout the system. One example of successful spread comes from Hartford HealthCare (HHC), an integrated health care system that has been a leader in the Age-Friendly Health Systems movement. Age-Friendly Health Systems is an initiative of The John A. Hartford Foundation and the Institute for Healthcare Improvement, in partnership with the American Hospital Association and the Catholic Health Association of the United States.
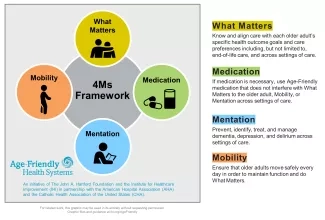
In Age-Friendly Health Systems, age-friendly care is defined as care that is based in the “4Ms”: What Matters, Medication, Mentation, and Mobility (see Figure 1).
For HHC, spreading age-friendly care means adopting the 4Ms throughout the system across its sites of care. HHC offers the full continuum of care with seven acute-care hospitals, behavioral health and rehabilitation services, and a comprehensive range of services for seniors. Hartford Hospital is the flagship hospital. Implementing age-friendly care was spearheaded by Christine Waszynski, APRN, Coordinator of the Geriatric Consult Service, ADAPT and NICHE Programs at Hartford Hospital, and Dr. Robert S. Dicks, MD, FACP, Director of the Geriatrics Programs at the hospital.
In September 2018, they started with a pilot in five units serving older adults at their flagship Hartford Hospital. When they had successes and shared their stories, other units took notice and expressed interest in learning. The work includes the SAFER mobilization program, cognitive and physical exercise programs, deprescribing, a delirium care pathway, and dementia screenings in primary care settings, among other interventions. “We start small, show the benefit, and expand it from there,” said Cheryl Ficara, RN, MS, NEA-BC, Senior Vice President of Operations, Hartford Region.
The Age-Friendly Health Systems initiative has identified the following drivers to help spread the 4Ms:
- Data: Collect quantitative and qualitative data from the start, both process and then outcomes data. Analyze all data by age, race, and ethnicity to try to ensure that the 4Ms are implemented equitably.
- Aim: Know from the start how far and by when you will spread the 4Ms. Find the balance between testing on a small scale and holding your larger aim and vision.
- What Matters: Find the strategic priorities advanced by the 4Ms. Make sure that you're clear on your organization's strategic priorities, what matters to the health system, and how the 4Ms can move that forward.
- Financial Impact: Financial well-being is part of what matters to the health system. Calculate the return on investment of the 4Ms in your hospital and practices. IHI offers ROI calculators and other tools to make the business case for the 4Ms in your system.
- Stories: Stories of people help drive change. Share stories with leaders so they have enough understanding and stories to be able to advocate for change.
These drivers have informed the work at HHC. One key for HHC was recognizing and highlighting how the 4Ms advanced their existing strategic priorities.
They have three overriding strategic priorities:
- Promote optimal wellness/recovery and eliminate patient harm (i.e., excellent outcomes)
- Provide optimal patient/family experience
- Support HHC staff
The 4Ms advance these priorities and make an impact on what matters to HHC. For example, the 4Ms work focuses on reducing falls with injury, sepsis, medication errors, and cognitive loss, among other goals. For patient and family experience, the age-friendly work involves promoting care in the optimal setting (home if possible), as well as providing patient and family education on prevention and management of geriatric syndromes. As for supporting the staff, the 4Ms work includes providing education on geriatric best practices to all clinical staff; instituting volunteer programs to support older adults; and providing resources such as sensory aids, mobility aids, and exercise equipment.
According to Christine Waszynski, “My colleagues, they want to do a good job with older adults. They are eager to learn, are eager for suggestions, but definitely need the support to be able to do some of the best practices that we read about and that we know about that work.” It’s the responsibility of leadership, she said, to “be sure they have the resources they need.”
HHC also benefits from a highly structured operating model. Every day, they hold interprofessional huddles, bedside handoffs, and rounds. They look at outcomes daily. In the pilot, they examined data every day to see what was working and what wasn’t working. Presence of and support from leadership were key. “That kind of structure helped us to take the concepts and the evidence-based practice of the 4Ms and embed it into our day-to-day work and embed it into the care of patients every day,” said Ficara.
This work has led to striking outcomes. The SAFER Mobilization program demonstrated a 43 percent reduction in falls over the first six months of implementation, along with an increase in episodes of patient mobilization. The ADAPT program (Actions for Delirium Assessment, Prevention and Treatment) led to a 40 percent overall reduction in delirium-attributable days over six years, averaging an 8 percent reduction per year. [Delirium-attributable days are defined as hospital days during which there are signs and/or symptoms of delirium as indicated by an abnormal assessment on the Confusion Assessment Method (CAM).]
HHC leaders make sure to share that data with other units and providers in the system, and to tell stories to celebrate and make the successes real. According to Ficara, these stories focus on each person’s humanity: “We made a difference for this human being. This is one less person who had to suffer from delirium. We transitioned this person to home in a very appropriate, family-centered way.”
That kind of storytelling is essential to motivating other units to get involved and ultimately to successful spread. “Making it real,” said Ficara. “That makes all the difference in the world.”
You may also be interested in:
Spreading Age-Friendly Care: From One Care Location to Reach Older Adults Across Your Health System
