Why It Matters

Source: Rush Photo Group
Why are we explicitly addressing the problem of health equity at Rush University Medical Center? Because, like a lot of academic medical centers, we serve people in one part of our city who don’t have great access to care. They often struggle with high unemployment, job scarcity, poverty, and other social determinants of health that contribute to health risks and poor outcomes. Then, on the other side of the city, people are employed, have regular access to health care, and generally have a better quality of life with longer life expectancy.
This is not theoretical or anecdotal. We look at our own data. We look at our own neighborhoods. We look at our own costs. People are often surprised at the striking inequities we identify.
For example, here’s what we learned when we mapped out life expectancy by neighborhood in West Side Chicago:
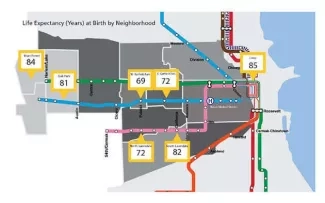
Source: 2016 Rush Community Health Needs Assessment
When we saw dramatic disparities in morbidity, mortality, and life expectancy within miles of one another, and identified ongoing health crises in the neighborhoods around us, we knew we had to act.
Finding these differences was no accident. We made a conscious effort to analyze the data for possible disparities, which required learning to look at data in different ways.
For example, we saw similar rates of diabetes between different populations. So, where’s the disparity? When you compare whose diabetes is controlled and whose isn’t, or whose condition is more severe, or who has access to insulin, the disparities become more apparent. We may be finding a similar incidence of diabetes, but certain neighborhoods have much higher rates of poor control and comorbid disease. The data, when you slice it open and take a closer look, show you where you should focus. The data drove us out into the community.
Seeing the Big Picture
When we look more closely, the data provide a narrative about how factors like substandard education and unsafe neighborhoods influence the health of the populations who live there. Our community health workers, who are there every day living and breathing it, validate the story and help provide nuance. With their help and with our patients, we’re now talking about how we can improve health inside the doctor’s office and outside. We’re addressing factors that we can control with a pill, and those that we cannot.
For example, screening our primary care patients for social determinants of health is helping us better understand our patients' lives. We began asking whether they have food, a place to stay every day, who in their family helps with their care, etc. There was a patient who was, at first, reluctant to respond to these personal questions. At the end of the screening, though, she revealed that she didn’t have a steady paycheck. She was living with a friend and didn’t know where to go next. This explained why she hadn’t been taking her medications. She left the room tearful, not because of the situation, but because she was finally able to share what was going on with someone who was interested in helping and had the resources to do so.
The key is that you must be prepared to act on the answers that people give you when you screen for social determinants of health. We are fortunate because we’ve partnered with an organization known as NowPow. They provide a curated set of resources that are available close to a patient’s home. When someone says they need help with food insecurity, for example, we place a direct referral that notifies the community organization that we have a patient in need, and we connect the person with food assistance. We then receive feedback confirming their needs were addressed.
A physician doesn’t have to be the one asking the screening questions or making all the referrals. Various members of our clinical teams, including medical students and community health workers can screen and connect patients with resources. Not everyone is aware of all the resources available, so it’s been great to work with an organization dedicated to putting them at people’s fingertips.
How to Start Using Data
One of the easiest ways to start using your data to further your health equity work is to take one clinical condition and a single, small population based on whatever data you have available. Then, look for patterns.
We looked at our data on cardiovascular risk factors. We found big disparities, not only regarding prevalence of disease, but how we were performing on quality metrics.
One cut at the data showed us that we weren’t doing well managing cardiovascular risk factors for men. There were similar rates of elevated Atherosclerotic Cardiovascular Disease (ASCVD) risk scores and missing documentation of risk factors, including not having their cholesterol checked or information about their smoking status. But when we looked more closely, we found significantly more men in black and brown communities who did not have their diabetes or blood pressure under control.
Once you determine where to focus your attention, you create a team to support that clinical workflow to address one or two of the relevant metrics. You also work together to figure out the structural barriers to good health for this population. A single physician can engage with a patient repeatedly, but if we don’t do anything about the social determinants of health that are getting in the way, we’re not really solving anything.
Understanding and using data should be at the heart of health equity work. You can’t address a problem if you don’t know it’s there, and you can’t assess your impact if you don’t measure it.
Facing Up to Racism
One of our biggest challenges is asking people to acknowledge that equity is a problem without personalizing it. We’re all proud of where we work and what we do, so it’s hard to admit that there’s racism in the structure of our organization, but it’s there and we need to address it.
We’ve learned from others who are part of IHI’s Pursuing Equity initiative about the value of addressing racism head-on to change organizational culture for the better. Following their example helped us bring discussions about health equity to our senior leadership. It’s now incorporated into our strategic plan.
The problem of structural racism evolved over many years, so it's not going to be fixed quickly, but we're determined to do something about it every day. And this includes the data analysts who work with our Pursuing Equity team. They know their work has the potential to change lives. It’s not just financial data, performance data, or data we submit to meet regulatory requirements It’s data for action.
Michael Hanak, MD, FAAFP, is Associate Chief Medical Information Officer at Rush University Medical Center. Rush University Medical Center is one of eight health care organizations taking part in the IHI-led Pursuing Equity initiative.
You may also be interested in:
IHI white paper – Achieving Health Equity: A Guide for Health Care Organizations
Facing Down Denial and Data Challenges When Addressing Equity
