Why It Matters

Photo by Greg Rosenke | Unsplash
In recent decades, the patient safety movement, the influence of regulatory and accreditation systems, value-focused management, and consumerism have highlighted the importance for health care organizations to implement a system for managing quality. While some organizations have made progress, many continue to address issues caused by poor quality without designing systems to prevent them altogether. A new white paper from the Institute for Healthcare Improvement (IHI) — Whole System Quality: A Unified Approach to Building Responsive Resilient Health Care Systems — proposes a more holistic approach to quality management. The following is an adapted excerpt from the white paper.
While health care organizations have made significant strides in improving the quality of care, health system leaders note persistent challenges in building resilient and responsive organizations that continuously, reliably, and sustainably meet the evolving needs of their communities.
IHI’s research on strengthening organizational resilience and responsiveness to patients and populations has been underway for a number of years. In a dramatic demonstration of how health systems are actively learning how to manage quality in new ways at an accelerated pace, the COVID-19 pandemic surfaced a number of emerging and evolving patient, provider, and community needs and forced health systems to quickly redesign care delivery to meet those needs.
Decades of scholarship, coupled with insights from the pandemic, reveal a way forward for health systems that are pursuing quality in health care: through a process of rigorous learning, health care organizations can design resilient and responsive management systems to continuously deliver services that reliably and sustainably meet the evolving needs of patients, populations, and communities — in times of both stability and crisis.
The Whole System Quality: A Unified Approach to Building Responsive Resilient Health Care Systems white paper proposes a more holistic approach to quality management — whole system quality — that enables organizations to close the gap between the quality that customers are currently receiving and the quality that they could be receiving by integrating quality planning, quality control, and quality improvement activities across multiple levels of the system. Whole system quality requires leadership principles and practices that foster a culture of learning to reliably and sustainably meet the evolving needs of patients, populations, and communities. The paper details how these leadership principles and management practices can enable health systems to pursue quality — with ambition, alignment, and agility — through a commitment to learning.
Significant Opportunities for Improvement
In the two decades since the Institute of Medicine published To Err Is Human: Building a Safer Health System, the health care industry has made great strides in improving the quality of care, including decreases in surgical site infections and hospital-acquired conditions, among other fundamental quality improvements. Despite these efforts, significant opportunities to improve health care quality remain, especially when considering the often unreported near misses. As Dr. Don Berwick noted, “[O]verall, so far as we can determine, the progress toward truly safer patient care remains frustratingly slow and spotty. Doing projects is not the same as transforming a system. Well-run airlines don’t rely on ‘safety projects.’ The scientific pursuit of safety infuses absolutely everything they do, all the time.” Pursuing quality holistically and embedding it into the health system requires positioning quality at the center of organizational strategy.
Today, quality in health care often means the attributes of products and services or conformance to requirements imposed by regulatory bodies. As Forbes’ Steven Denning describes, “All too often quality management in its various forms and labels has come to mean improving quality in the sense of internal processes, and conformity to internal specifications. In a word, bureaucracy. All too often in quality management, the customer has seemed to be the last thing on anyone’s mind.”
This reality would surprise the early quality theorists, whose work defined quality in terms of meeting customer needs. Deming introduced the concept of “customer-orientation,” and Juran integrated this idea with the notion of meeting specified requirements to propose his view of quality as “fitness for use,” comprising two elements: “features of products which meet customer needs” and “freedom from deficiencies” (see Figure 1).
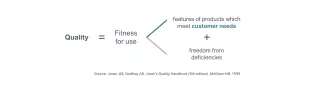
Figure 1 — Juran’s Definition of Quality
Source: Juran JM, Godfrey AB. Juran’s Quality Handbook (5th edition). McGraw-Hill; 1999.
Building on the ideas of quality movement pioneers, IHI proposes a strategic definition for health care quality: the endeavor of continuously, reliably, and sustainably meeting customer needs. This definition places quality at the center of the health care enterprise: quality is the organizational strategy, not merely a component of the strategy.
Like many complex organizations, health systems must consider the often-competing interests of myriad stakeholders to inform their strategy. To offer a clarity of purpose to organizational leaders, influential management theorist Peter Drucker proposed a useful distinction between primary and secondary customers:
- Primary customers: Individuals whose lives are changed by pursuing quality. In the context of health care organizations, primary customers are defined as the health care workforce, patient population, and community members who are current or prospective consumers of health care services.
- Secondary customers: Individuals whose engagement is necessary to deliver quality to the primary customers. In health care organizations, secondary customers include payers, partners, regulatory bodies, and accreditation agencies, among others.
To read about how whole system quality links to customer needs, organizational vision, and quality strategy, download the free IHI white paper.