Summary
- Whether it is managing a flight of stairs, going grocery shopping, or walking the dog, mobility is the foundation for living a healthy and independent life and supporting it is a crucial part of age-friendly care.
A dog can be more than “man’s best friend.” In the life of an older adult, for example, spending time with a beloved pet may be the motivation that helps them regain their independence.
Cynthia Brown, MD, MSPH, Chair of the Department of Medicine at Louisiana State University Health Sciences Center, knows this from experience. She is an expert on mobility and older adults. In a recent interview with the Institute for Healthcare Improvement (IHI), she shared the story of an older adult who, after being bedridden during an illness, was having difficulty walking from his bed to the hospital room door.
When asked what was important to him, the patient shared that he enjoyed walking with his dog around the block. Using this information as a source of inspiration, his care team explained that working with the physical therapists and nurses on his walking would be the key to returning to the activity that meant so much to him. He began mobilizing with hospital staff, walking further every time. Brown noted that even when hospital staff were unavailable, the older adult would march in place until he became tired. Months after his hospitalization, the patient continued working on mobility and was eventually able to get back to taking his dog for walks.
This is an example of why linking What Matters to other components of age-friendly care is so crucial. Brown is faculty for Age-Friendly Health Systems (AFHS), an initiative of The John A. Hartford Foundation and IHI, in partnership with the American Hospital Association and the Catholic Health Association of the United States. To be an Age-Friendly Health System means reliably providing a set of four evidence-based elements of high-quality care, known as the “4Ms,” to all older adults in your system: What Matters, Medication, Mentation, and Mobility.
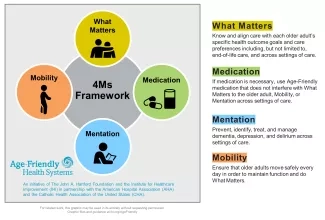
Figure 1. 4Ms Framework of an Age-Friendly Health System
Often, What Matters to older adults consists of maintaining independence, spending time with loved ones, or continuing hobbies or other pursuits they enjoy. “We want to help the older adult [continue] these activities,” Brown noted. “So, think about what mobility is required to achieve What Matters to them.” The goal of the mobility “M” is to encourage older adults to pursue their key objectives. Tangible goals can range from going to the mailbox, walking in the mall, or attending events.
Mobility does not only involve walking. Instead, “mobility is an activity that should happen at the patient’s or the person’s level, whatever they are capable of doing,” Brown explained. Wheelchair users may continue to mobilize by propelling themselves when doing activities. Even older adults confined to their bed can mobilize by moving around in their bed and rolling over on their own.
Evaluating Mobility
To improve mobility evaluation and make it more age-friendly, AFHS has developed a one-page collection of Age-Friendly Mobility Assessment Tools to assess mobility in a variety of care settings. Qualitative information achieved through observation can help with assessment. For example, watching the older adult get up from a chair without using their hands and observing the steadiness of their walk, ability to turn, and sit back in the chair can help inform an evaluation. For health systems reviewing their mobility assessment, Brown encouraged choosing a measure that is manageable within their setting and conferring with health care team members to encourage investment in the evaluation process.
According to Brown, a clinician should always evaluate mobility rather than relying self-report measures. She noted that patients may not be as concerned with certain aspects of mobility that may be crucial for a clinical assessment. For example, a patient might forget to mention that they have made modifications like grab bars in their shower or not realize the significance of dizziness, unsteadiness, or falls or near falls. Patients may also inflate their capacity for mobility or may not be reliable informants if they are cognitively impaired. Without a proper evaluation, the patient is less likely to receive adequate care and may be at higher risk for falls and decreased mobility.
The Unintended Consequence of Focusing on Falls
Evaluating the risk of injury from falls differs from assessing for mobility. Mobility evaluations are more challenging and harder to quantify than falls. The pervasiveness of fall risk evaluations has led to the sometimes inappropriate and potentially harmful limiting of activities and mobility of older adults in a well-meaning attempt to keep them safe.
To lessen the unintended consequences of prioritizing fall prevention, older adult care should focus on safe mobility, Brown advised. Promoting safe mobility for older adults includes removing or otherwise addressing safety risks in the home (e.g., throw rugs, cords on the floor, or pets) and assessing an older person’s physical strength and support system. Ensuring safe mobility helps to keep an older adult active and mobile while supporting fall prevention.
Whether it is managing a flight of stairs, going grocery shopping, or walking the dog, mobility is the foundation for living a healthy and independent life and supporting it is a crucial part of age-friendly care. Understanding What Matters to patients and creating a reliable system for mobility evaluation are the keys to meeting the challenges of evaluating and promoting safe mobility.
Luisana Henriquez Garcia is an IHI Project Manager.
Photo by Binomialphoto | flickr | Image licensed under the Creative Commons Attribution-NonCommercial-NoDerivs 2.0 Generic license
You may also be interested in:
To have more efficient, effective, and productive appointments, share this new guide, My Health Checklist, with patients before they come in.
On April 10, 2024, the Centers for Medicare & Medicaid Services (CMS) proposed the Age-Friendly Hospital measure. It encourages hospitals to improve care for patients aged 65 years or older. You can show your support for this important measure to improve the quality of care for older adults by leaving a comment before Sunday, June 2, 2024. For more details: Age-Friendly Attestation Measure in the Federal Register.
