Why It Matters

Photo by PNW Production | Pexels
The CDC’s Pregnancy Mortality Surveillance System presents sobering statistics related to maternal mortality in the US and existing disparities. Updated research on maternal deaths in the US from 2016-2017 found that the maternal death rate among non-Hispanic Black women was 3.5 times greater than the rate among non-Hispanic white women, contradicting previous research that had calculated a 2.5 times higher death rate for Black women. The postpartum period presents an important opportunity to intervene before outcomes recur or worsen later in life and/or with future pregnancies (e.g., later cardiovascular disease or diabetes).
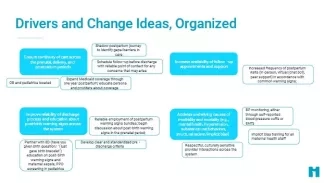
In preparation for the launch of the IHI Eliminating Inequities and Reducing Postpartum Morbidity and Mortality learning community, we conducted a 90-day Innovation cycle to answer the following question: What interventions and related measures can hospital systems test to reliably improve postpartum care and equity for people who give birth? We identified four key areas for intervention, which may inform the improvement projects undertaken by the learning community participants:
- Reduce variability, particularly in discharge education practices and post birth warning signs—strive for consistency for the entire patient population, and measure what was learned, not just delivered;
- Offer implicit bias training for all staff;
- Forge deep partnerships to understand implementation challenges specific to partner organizations and to better understand what birthing persons want and need in the immediate postpartum period;
- When possible, partner with Emergency Medicine, Behavioral Health, and Pediatrics to promote continuity of care.
Our research methods involved literature scanning and qualitative interviews with experts in the field. Approximately 10 organizations were represented in our interview list.
Source: Institute for Healthcare Improvement Innovation Team
Through our interviews, we heard that many clinicians remain unaware that the US is facing a maternal health crisis, meaning that raising awareness is a vital component of the work ahead.
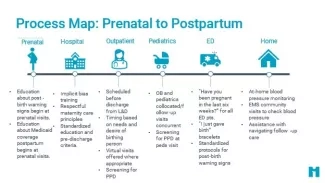
Discharge Process
We heard that many serious health events and deaths occur in individuals whose vital signs were not completely normal when they were discharged from the hospital after giving birth—elevated blood pressure, slight fever, etc. Standard pre-discharge criteria and concerted follow-up could help avert some of the adverse outcomes. The discharge process is highly variable, both between and within institutions.
Post-Birth Warning Signs and Post-Delivery Emergencies
ED staff should be trained to ask women awaiting triage whether they have been pregnant in the last six weeks, thereby alerting them to potential pregnancy and birth-related complications. Cardiovascular symptoms may present atypically post-delivery and can therefore often be missed and cause major—potentially catastrophic—delays in receiving appropriate treatment.
Education on post-birth warning signs, along with assessment, should begin in the prenatal period and should be standardized for all patients, perhaps using an EHR-based checklist to minimize the impact of unconscious bias on care. Those responsible for offering this education should consider not only what material is covered but when and how it is delivered (e.g., waking a patient up before dawn to review post-discharge instructions is not equivalent to approaching her when she is already awake and has eaten.
Follow-Up
Models of care that incorporate doulas are widely touted and contain elements of an ideal design, but financial barriers for many patients and staffing constraints pose challenges to scale up. In addition, apps and startups focused on the postpartum period, while novel, are not currently integrated with the health care system and do not appear to be closing the equity gap.
Patient navigators can be enlisted to forge community connections and maintain contact with patients in the postpartum period. However, these sorts of programs do not have an obvious funding source and may need to be self-funded by the health care organization(s) choosing to pilot them.
New mothers are likely to be overwhelmed by tending to a newborn’s needs, and they might not prioritize their own follow-up care. We heard that, since virtual visits often have higher attendance, making them an option more frequently could be beneficial. Similarly, co-locating OB care and pediatric care offers one-stop shopping for mothers and newborns.
Patient-Centered Design
Some interviewees expressed concern about patient-centered design and co-designing new interventions. For instance, we heard that patients should have their postpartum follow-up visit scheduled prior to their being discharged from the hospital, and the visit should be scheduled in a time frame that meets the patient’s needs, rather than conforming to a visit schedule. Relatedly, some regions and Medicaid agencies are opting to add a postpartum visit at 1-3 weeks post-delivery (rather than waiting until the standard 6 weeks), but interviewees expressed some concern that this decision is neither being co-designed with patients nor considering what people who have just delivered might want and need.
Source: Institute for Healthcare Improvement Innovation Team
What’s Next: Testing with Health Systems
Five birthing hospitals were selected through a competitive application process to join a Learning Community with IHI, which began in January 2023. During this 6-month engagement, participating hospitals will evaluate their available data, map out current processes for postpartum care, and develop a deeper analysis of “what matters to you” for birthing persons, with a focus on improving care and outcomes for Black women. This will help us build on the key areas for improvement identified in the innovation cycle, as well as determine high impact levers and opportunities to improve access to and experience with postpartum care and support.
Deborah Bamel, MPH, is an IHI director. Marian Johnson, MPH, is an IHI faculty member. Marina Renton, MPhil, is an IHI research associate. This project is funded by Merck for Mothers, Merck’s global initiative to help create a world where no woman or birthing person has to die while giving life.
You may also be interested in:
Better Maternal Outcomes Quality Improvement Workbooks — Contain examples and templates to guide QI work focused on improving maternal health outcomes and equity
Black Maternal Health: Reducing Inequities Through Community Collaboration
