Why It Matters
One of the keys to providing safe, high-quality health care is implementing best practices for every patient, every time. Carrie Rubenstein, MD, understands this. Rubenstein is a family physician, geriatrician, and clinician educator who directs the Geriatric Assessment Clinic at Swedish Health Services (Seattle, Washington). Since being selected to participate in the American Hospital Association (AHA) Next Generation Leaders Fellowship, she has been leading a pilot project to measure how reliably the Age-Friendly Health Systems “4Ms” framework is being implemented (see Figure 1) along with a 5th “M” (Malnutrition) the team added to reflect the importance of proper nutrition and food security for older adults.
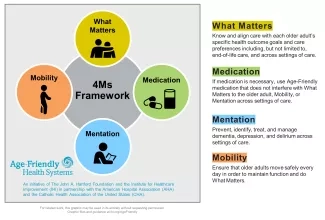
Swedish Health Services is the largest nonprofit health care provider in the greater Seattle area and is affiliated with Providence Health & Services. Providence was one of five pioneer health systems in 2018 to join Age-Friendly Health Systems (AFHS), an initiative of The John A. Hartford Foundation and the Institute for Healthcare Improvement, in partnership with the AHA and the Catholic Health Association of the United States.
For the pilot project, the team chose a representative metric for each of the 4Ms (plus Malnutrition). They included these measures in the template for their geriatric assessment. For each visit, the goal was to assess the 4Ms plus Malnutrition using one of the selected evidence-based methods:
- What Matters — The team asks every older adult, “What matters most to you?” They also ask whether the older adult has a trusted decision maker. The answers are recorded in the “goal of care” note, a tool within the electronic health record (EHR). It is also possible to include the story behind What Matters in the EHR and document additional care preferences.
- Medication — The team’s pharmacist does a one-on-one medication reconciliation with each older adult. The pharmacist identifies high-risk medications and discusses opportunities for deprescribing. “Deprescribing is a key focus of the geriatric assessment clinic,” said Rubenstein. “Many elders want to be on fewer medications, and it takes time to identify those medications that may not be necessary and discuss safe ways to safely deprescribe.”
- Mentation — To assess mood, the team administers the Patient Health Questionnaire-2 (PHQ2), a brief depression screening, or the Geriatric Depression Scale (GDS), a 15-question test for older adults. Which assessment they use depends on a variety of factors, including the patient’s condition and the amount of time available. They also administer one of three cognitive assessments: the Mini-Cog, the MoCA, or the RUDAS. It is common for an individual to receive a first diagnosis of dementia during this geriatric assessment visit. Disclosing the diagnosis of dementia takes time, skill, and sensitivity. Rubenstein and her team share recommendations with the older adult’s primary care physician and see the older adult and their care partner three to six months after the initial visit to follow up.
- Mobility — The team administers the Timed Up and Go (TUG) assessment and the Stopping Elderly Accidents, Deaths & Injuries (STEADI) screening for falls prevention. They also do a functional assessment of every older adult using the Lawton-Brody Instrumental Activities of Daily Living (ADL) scale or the Katz Index of Independence in Activities of Daily Living.
- Malnutrition — The team administers a simple screening for unintended weight loss and food insecurity. For the latter, they use the Hunger Vital Sign™ assessment. “Food insecurity is one of those topics that people don’t talk about but is likely far more critical to the health and well-being of the people we care about than other topics we spend considerable time and energy on,” Rubenstein noted.
Rubenstein observed that the AFHS framework represents aspects of care the team was already delivering, but adhering to the 4Ms framework (plus Malnutrition) has helped ensure that the clinicians address all of them every time. Rubenstein also appreciates the utility of the 4Ms framework for teaching. It helps simplify the care “in a digestible way to understand the factors that we believe are so critical,” she said.
Challenges and Opportunities
The COVID-19 pandemic disrupted Rubenstein’s project just as it was getting started. To adapt, the team asked themselves, “What is essential?” and “How do we provide essential services in the safest way possible?” and experimented with a variety of combinations of in-person and virtual meetings and exams.
Rubenstein knew that the pandemic added challenges to those already faced by their patients. “People were going to be more isolated,” she observed. “There would be an impact on mentation and mobility.” On the upside, “There was an opportunity for preventing the potential outcomes that we knew older adults were at risk for.” For example, they started a grocery delivery project. They secured funding from the Swedish Foundation to bring $200 grocery deliveries to 100 patients they identified as high-risk.
Impact
The team did a chart review for 31 visits from November 2020 to February 2021. They found that 67 percent of visits had documentation of What Matters or advance directives. A depression screening was administered during 61 percent of visits, and a cognitive screening was conducted during 74 percent of visits. In 100 percent of the visits, the patient was screened for fall risk with the STEADI tool; the pharmacist performed a comprehensive medication review and identified high-risk medications; and screenings were completed for unintended weight loss and food insecurity.
In February 2021, the clinic gained the Level 2 Committed to Care Excellence certification from AFHS. This recognition is given to teams that have collected three months of verified data demonstrating the early impact of using the 4Ms.
Looking Ahead
The team plans to continue refining the measures for assessment of the 4Ms plus Malnutrition and to integrate this work into their documentation and reporting practices. For example, Rubenstein has to open every chart individually to collect age-friendly data. “We need to make this easier and more efficient for my colleagues,” she noted. “We need to give them the right tools, make them accessible, and measure this in the most efficient way.” This will mean optimizing the electronic health record (EHR) to create an “age-friendly snapshot.”
In April 2021, Rubenstein presented at the first Providence Age-Friendly Health Systems Symposium. That system-wide kick off launched an Age-Friendly Innovation Challenge with 40 entries. Each participant will compete for grant money to implement age-friendly endeavors throughout Providence Health.
“Playing a leadership role in helping Swedish and Providence in the Age-Friendly Health System journey has been a meaningful and satisfying addition to my work,” said Rubenstein. “I believe that through this age-friendly journey, we can have a tremendous impact on the care of older adults, the experience of care partners, and the satisfaction of care providers and care teams.”
Editor’s note: This post was adapted from an article about the American Hospital Association Next Generation Leaders Fellowship to be published soon.
You may also be interested in:
