Why It Matters
Photo by NEC Corporation of America with Creative Commons license
Each year, hundreds of older adults end up in the hospital at Banner Health in Phoenix, Arizona after experiencing a fall. About 20 percent of all visits to the emergency department are by older adults. Of these, about 10 percent (approximately 1,200 patients) resulted from a fall. Harm from falls represents one of many opportunities for improvement that Banner Health’s Division of Geriatric Medicine is determined to address.
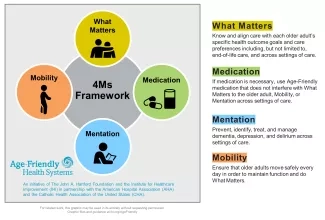
Banner Health is one of the largest nonprofit health care systems in the country. In 2019, Banner University Medical Center in Phoenix joined Age-Friendly Health Systems (AFHS), an initiative of The John A. Hartford Foundation and the Institute for Healthcare Improvement (IHI), in partnership with the American Hospital Association and the Catholic Health Association of the United States.
“We were on the Age-Friendly Health System bandwagon pretty early on,” said Nimit Agarwal, MD, associate professor at Banner University Medical Center and Director of the Division of Geriatric Medicine. Age-Friendly Health Systems define age-friendly care as care based on the “4Ms”: What Matters, Medication, Mentation, and Mobility (see Figure 1).
In 2017, Agarwal and his team implemented a model called virtual acute care for elders (vACE), which involves daily rounding on patients who are 70 and older on the medical-surgical floor. Conducted via a widely available virtual meeting platform, the rounds are led by a geriatrician and attended by an administrative assistant, a nurse leader, a case management leader, a pharmacy leader, and a therapy leader. The team reviews data in the electronic health record (EHR), including reason for visit, living situation, ability to perform activities of daily living prior to admission, completion of advance directive, distance walked yesterday, distance of fall, and the results of 4Ms screenings.
Initially, the team was evaluating mobility without seeing expected improvements. “We were using the Bedside Mobility Assessment Tool (BMAT), but there was no intervention connected to it,” said Agarwal. Once they realized this, they started to assign corresponding interventions for each score on the BMAT. For example, patients who score a 1 dangle their legs over the edge of their bed for 5 to 15 minutes, three times per day. Those who are more mobile, scoring 3 or 4, walk at least 150 feet three times per day.
The team uses an early mobility dashboard that tracks process measures. One tool reminds nurses every three hours to check whether a patient has performed their designated intervention. The dashboard also helps leaders see progress on the unit, hospital, and health system levels.
To address the mentation element of the 4Ms, nurses administer the Brief Confusion Assessment Method (bCAM) twice per day for each patient. However, for various reasons, the delirium detection rate with this tool has been low. So, instead of relying only on the bCAM, Agarwal’s team decided to ask nursing staff to input additional data several times a day in the EHR: neurological assessment, verbal assessment, and patient orientation. If any of these variables are positive, the nurses do a more thorough assessment. “It’s kind of an early warning system,” said Agarwal.
The virtual rounds have led to improvement in delirium detection, reductions in days with indwelling catheters, improved mobility, increased geriatric palliative care utilization, and higher rates in identifying a surrogate decision maker.
The trauma service at Banner Health was inspired by the results of the vACE rounds. They now conduct trauma acute care for elders (TrACE) rounds.
The Geriatrics Division’s palliative care team uses the 4Ms to guide care for all their patients. “We know that early palliative care consultation helps improve outcomes for patients,” said Agarwal. For patients 65 and older, the team tracked how long it took to complete an initial palliative care consultation after the patient’s date of admission. They found it was an average of 4.47 days. This was almost three days earlier than the usual palliative care team consult. “This is the value of the vACE and TrACE rounds — to identify these high-risk patients early,” said Agarwal.
They also compared length of stay for patients receiving 4Ms geriatric palliative care with patients receiving the typical palliative care and saw an almost one-day difference for every risk category: low, moderate, high, and severe. This translates into reduced costs.
In January 2020, Banner University Medical Center was recognized by AFHS as Committed to Care Excellence. “We are very excited with these results,” said Agarwal. “We are hoping we can continue to look at these measures, look at some of the outcomes, and expand clinical outcomes throughout our health care system.”
You may also be interested in:
Using the Age-Friendly 4Ms to Better Advocate for Older Adults (and Geriatric Care)
