Why It Matters
The debriefing facilitator’s request to debrief after the case was met with perplexed faces. “Why?” the team leader asked. “We had a great outcome and things ran smoothly. I wouldn’t have done anything differently.” The team had successfully stabilized a serious trauma patient, completing multiple complicated interventions simultaneously with prioritized precision, clear communication, and overall excellent teamwork. Not surprised by the response, the facilitator gathered the team. It quickly became apparent that one team member was averting his gaze. As the debriefing progressed, he was encouraged to share his reaction to the case. He shared that he was upset about a similar case earlier that week when he was unable to successfully complete a particular procedure. Multiple team members spoke up to normalize the situation, sharing their own experiences with struggles in complicated cases and the reality that sometimes things do not go as smoothly as the present case. Seemingly reassured, the team member then offered his perspective on why that task had gone well in current case. The team identified lessons that were broadly applicable. The debriefing concluded seven minutes after it began.
Health care debriefings are collaborative, reflective conversations following a simulated or clinical event. Debriefing is a powerful way to capture the knowledge and adaptations of frontline health care workers and facilitates understanding of system resources and constraints. Debriefing has been demonstrated to improve performance and clinical outcomes, and their use aims to enhance critical thinking and improve future clinical practice.
Debriefings are most commonly conducted to analyze events and maximize quality improvement, patient safety, and overall culture of safety. For example, Rose and Rose (2018) implemented a novel process for utilizing debriefing checklists to improve value in surgical care that resulted in debrief-driven improvements such as reduced proportion of surgical cases with reported defects, significant reduction in the 30-day unadjusted surgical mortality, lowered costs, and better workforce safety climate. Debriefings after in-situ simulations done in the real clinical environment — as opposed to a simulation center — have been utilized to identify knowledge gaps, reinforce teamwork behaviors, and identify previously unreported safety threats, such as malfunctioning equipment and knowledge gaps concerning role responsibilities among health care workers.
Debriefing methods have been largely adapted from aviation and psychology and there are many models of both post-simulation and clinical event debriefing. Multiple studies also indicate there is no one right way to debrief. Published debriefing models all tend to have these core components:
- Establishment of psychological safety
- Elicitation of reactions
- A case description
- Analysis of the event(s)
- Summary
Debriefing can take place immediately after the conclusion of an event, at the end of a shift, or during a future meeting. Though debriefing can include the presence of a trained facilitator, teams can also self-debrief using debriefing scripts and cognitive aids.
During debriefing, team members gather to discuss the case details and collaboratively review their actions, thought processes, and clinical reasoning. They discuss areas of strength and opportunities for improvement. Discussion may be broadened to include comparable cases with similar or different outcomes and how team actions and thought processes compared.
An often unseen benefit of debriefing can — and should be — debriefing for the wellness of the health care workforce participants. Quality, culture of safety, and wellness are inextricably linked, and debriefing is a way to address all three (as highlighted in Figure 1 below). No one can fully engage in discussions around maximizing patient safety and quality while in distress, and no one in distress from their health care experiences can truly heal without debriefing, a forum to be heard, and sharing their perspectives and ideas.

Figure 1 — Healthcare Debriefing: Linking Quality, Safety & Wellness
Debriefing serves as a “safety net” in many ways. It is a proactive way to uncover opportunities for improvement, including latent safety threats that may be mitigated before harm occurs. Furthermore, debriefing can serve to identify participant stress and need for additional support, related or unrelated to a specific case. This allows facilitators to refer individuals to available programs, such as peer-support programs and cadre of available wellness resources. Debriefing also serves as a forum for conflict resolution if there is disagreement during a case. Rather than ignoring differences, it supports open dialogue between team members, allowing all to share their unique perspectives and areas of concern.
Learning From All Types of Events
Historically, health care safety science has focused predominantly on reducing risk and minimizing harm by learning from when things go wrong (Safety-I). The use of debriefing is often used in health care after high-stakes events (e.g., cardiac arrest resuscitation, postpartum hemorrhage, or trauma care) or unfavorable outcomes.
While debriefing and learning from “positive” events is routine after simulations, both simulation and clinical event debriefing programs are often more focused on Safety-I debriefing. While some published debriefing frameworks include analysis of favorable outcomes, they do not include a guide to delve into the factors contributing to positive performance. This includes exploring specific Safety-II concepts such as adaptation, resource utilization, and workarounds to harness the power of everyday work-as-done (versus work-as-imagined, e.g., protocols). Developed through expert consensus, we propose the Safety-II Healthcare Debriefing Tool (see Figure 2 below).
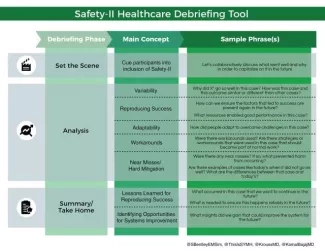
Figure 2 — Safety-II Healthcare Debriefing Tool
Using the Safety-II tool will encourage review of all events, including the most routine, because there is so much to gain from debriefing all case types. This will allow for analysis and reinforcement of why, in most cases, things go well. Also, if facilitated discussion and review became the norm after all cases regardless of outcome, debriefing would very likely shift from what often feels punitive and stigmatized — or even dreaded — to a welcomed and productive post-event conversation. Debriefing positive outcomes would also allow health care workers to use relatively low-stakes situations to develop their ability to share insights and prepare them for more difficult post-event conversations.
More debriefing would greatly benefit workforce wellness and health care quality and safety. Debriefing inclusive of Safety-II sets the stage for debriefing any type of event or outcome, primes teams to debrief more, and prepares them for debriefing after a particularly emotionally charged or unfavorable event. Debriefing inclusive of Safety-II may teach us how best to support learning and wellness during debriefings of the hardest, saddest, or most challenging cases.
Suzanne Bentley, MD, MPH, FACEP (@SBentleyEMSim), is the Medical Director of the Elmhurst Satellite Simulation Center, New York City Health + Hospitals/Elmhurst. Simon Huang, MD (@ThisIsSYMH), is a Royal College of Physicians and Surgeons emergency medicine resident, Dalhousie University. Mona Krouss, MD, FACP, CPPS (@KroussMD), is Director of Patient Safety, New York City Health + Hospitals. Komal Bajaj, MD, MS-HPEd (@KomalBajajMD), is Chief Quality Officer at NYC Health + Hospitals/Jacobi.
Photo by Edge2Edge Media | Unsplash
