Why It Matters
Racism and other forms of oppression are causes of health inequities that are often difficult to identify at first glance. Eliminating inequities requires digging deeply into the entrenched policies, practices, and culture of an organization and uncovering often uncomfortable truths. Addressing clinical inequities is one essential way health care organizations can improve health and health care equity for the populations they serve. The following is an excerpt from Improving Health Equity: Eliminate Racism and Other Forms of Oppression, one of five IHI guides describing strategies and lessons learned from the health care organizations participating in the Pursuing Equity initiative.
Health care organizations need to understand how their clinical operations are contributing to equitable care (or not) and ensure that equity is included as a key component of care quality. A focus on equity entails decreasing gaps in equity, with a particular emphasis on marginalized populations, while also improving care systems for all populations.
As noted in some guidance for health care leaders, “Quality improvement often focuses on populations where success is most easily achieved. But if we are going to start reducing disparities, we need to start with the ‘last’ population — one that may be more challenging and just not thriving — and partner with them to develop improvements. The reward for health care organizations is that even though these populations may be small, they can incur great costs to the health system. And if we can solve problems for those at the margins, we may come up with solutions that work better for all.”
Improving clinical processes and outcomes to improve equity for all includes stratifying quality data by race, ethnicity, and language (REaL) and by socioeconomic status/income, as well as working to reduce inequities and improve overall clinical processes. Health care organizations also need to look at access to services stratified by these same factors, to ensure that people of color have equitable access to all services provided, including high cost procedures such as cardiology services, hip and knee replacements, and bariatric surgery, for example. It is not enough to identify racial inequities in care for those who have managed to access to the system. The organization needs to proactively ensure that all populations, particularly marginalized ones, have equitable access to services.
Identify Where Equity Gaps Exist in Clinical Outcomes
Pursuing Equity teams tested the following changes:
- Integrate an equity lens into existing clinical dashboards that stratifies data for key measures by REaL factors.
- Design and utilize a specific equity dashboard, which is a distinct product that complements other dashboards. An equity dashboard might feature data for measures where the largest inequities exist, whereas a dashboard with an equity lens contains typical clinical quality measures stratified by REaL factors.
- Distribute reports containing data on equity gaps to clinical providers.
- Implement a process to provide on-demand stratification of requested clinical data by REaL factors.
For additional information on building data infrastructure and equity data displays and dashboards, see the guide for the second component of the IHI framework, Build Infrastructure to Support Health Equity.
Example of changes tested:
- To develop the most effective equity dashboard, in the design process the team at Rush University Medical Center in Chicago asked several key questions: Who is the dashboard’s intended audience? What are users trying to accomplish using the dashboard information? How will we know that the dashboard is helping users achieve their aims?
The initial version of the equity dashboard was used by Rush’s Pursuing Equity team, which included a senior leadership sponsor, physician champions, population health practitioners, quality and performance improvers, IT managers, and representatives from the Rush Center for Community Health Equity. The team selected four ambulatory clinical measures (diabetes, breast cancer screening, colorectal cancer screening, blood pressure) and then stratified data for these measures by race, ethnicity, language, and zip code (see Figure 3). The team tested and refined the equity dashboard using multiple iterative Plan-Do-Study-Act (PDSA) cycles to evolve the dashboard from an initial wireframe, through multiple draft versions, and then to a final dashboard that was shared and used more widely throughout the organization.
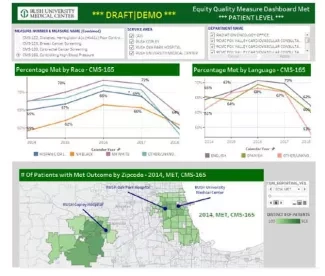
Figure 3. Example Equity Dashboard from Rush University Medical Center
Use Quality Improvement to Narrow Equity Gaps
Pursuing Equity teams tested the following changes:
- Stratify clinical process and outcomes data by REaL factors to identify where gaps in care exist.
- Based on this data analysis, initiate quality improvement efforts to narrow gaps in identified areas (e.g., emergency department admissions, complete childhood vaccination, routine medical procedures and screenings such as colorectal cancer screening and mammography).
Example of changes tested:
- The Brigham and Women’s Department of Medicine (DOM) team identified equity gaps in the treatment of and outcomes in congestive heart failure (CHF) patients, a condition that accounts for the highest number of medical discharges in their hospital. Research initiated through the DOM Health Equity Committee documented differences in access to specialty care and the impact on readmissions rates for CHF patients. Patients receiving inpatient treatment under medical team coverage had poorer outcomes and higher readmissions rates; patients receiving treatment under cardiac team coverage had better outcomes (see Table 1).
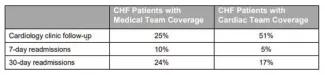
Table 1. Brigham and Women’s Hospital CHF Patient Outcomes: Medical Team vs. Cardiac Team Coverage
By analyzing their data, the Brigham and Women’s team identified that white patients are more likely to be admitted under the care of a cardiac team than patients of color, older patients, and women, creating a gap in equitable care. This gap is compounded by the fact that CHF is known to have a higher prevalence and incidence in black patients, who are 1.5 times more likely to develop CHF than white patients.
The Brigham and Women’s team sought to identify the structures and processes contributing to this equity gap and address it by standardizing patient bed assignment processes; engaging emergency medicine, cardiology, general medicine, and the heart failure service; improving heart failure care on the general medicine service; eliminating discrepancy in cardiology clinic discharge follow-up between medicine and cardiology services; and addressing structural drivers of inequity. In addition, it was critical that, as a team, they had a shared analysis of this as a systems issue and an example of race-based advantage leading to inequities.
Break Down Silos to Motivate Clinical Teams to Work Together
Pursuing Equity teams tested the following changes:
- Transparently share clinical data stratified by REaL factors with clinical teams.
- Attend trainings together to gain a shared understanding of racism and other forms of oppression so clinical teams can work together from a shared foundation.
- Present equity data and information in meetings with clinician groups.
- Include quality improvement staff in equity improvement efforts and teams.
Example of changes tested:
- To reduce silos and provide strategic guidance, Henry Ford Health System in Detroit, Michigan, launched a health equity steering committee comprising senior leaders, including the Senior Vice President for Population Health and the Chief Medical Officer of Primary Care, day-to-day team members, and equity content experts. The committee is co-chaired by the Senior Vice President of Community Health & Equity and Chief Wellness & Diversity Officer, and the Chief Quality Officer. The committee works with the equity and community health, quality and safety, and population health teams to focus specifically on how these teams can align strategies to improve health equity.
Below are some proposed measures to assess progress in this area:
- Percentage of clinical outcome measures reported to the board that are analyzed for differences using REaL data
- Percentage reduction in equity gaps over time for the same board reported clinical outcome measures stratified by REaL data
- Stratify the top three income-producing clinical procedures by REaL data to identify potential inequities
To see more lessons learned, resources, and examples, download all the Improving Health Equity: Guidance for Health Care Organizations publications.
You may also be interested in:
White paper — Achieving Health Equity: A Guide for Health Care Organizations
