Why It Matters
 Photo by the National Institute on Aging | flickr
Photo by the National Institute on Aging | flickr
Asking a patient what matters to them can be a deceptively simple way to prioritize often all-too-brief clinical encounters. Originally, some MaineHealth primary care providers had the question embedded within their system’s Medicare Annual Wellness Visit (AWV) template, but it was not at the top. Using a Plan-Do-Study-Act (PDSA) cycle to test optimal sequencing, they tried having the providers ask the question first.
According to Molly Anderson, Director of Geriatric Programs at Maine Medical Center (MMC), asking what matters at the beginning can helpfully guide the appointment. “The point we make is that it saves time,” she said. “You don’t have patients waiting and saving their agenda for the end of the appointment, saying, ‘Oh, wait, I forgot to mention something,’ or ‘One more thing.’” For busy providers, learning that asking about a patient’s priorities at the outset could save time — rather than lengthen a visit, a common concern — was crucial to winning the support of those who were unsure of the value of asking what matters.
“And then,” said Anderson, “they actually loved the conversations it elicited.”
MaineHealth has learned many such lessons about providing the best care possible for older adults across the care continuum in the last few years. Roughly one in five Maine residents is an older adult, and many of them receive health care from MaineHealth, a not-for-profit integrated health system that serves the state (as well as neighboring New Hampshire) through its 12 community hospitals, numerous primary care and specialty care practices, and comprehensive long-term care and senior care services. Over the next decade, MaineHealth hospital discharges for patients ages 65+ are projected to increase by 11.8 percent.
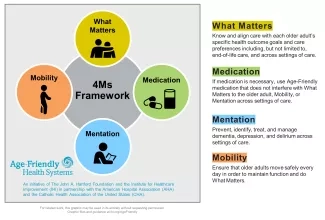
In 2018, to serve this growing population, MaineHealth joined Age-Friendly Health Systems (AFHS). AFHS is an initiative of IHI and The John A. Hartford Foundation, in partnership with the American Hospital Association and the Catholic Health Association of the United States. In Age-Friendly Health Systems, age-friendly care is defined as care that is based in the “4Ms”: What Matters, Medication, Mentation, and Mobility (see Figure 1).
MaineHealth was a member of the first AFHS action community. Since then, they have been piloting age-friendly care at several different levels — inpatient, long-term, and outpatient/ambulatory — and spreading the 4Ms throughout the system.
The team started with inpatient settings at Maine Medical Center (MMC), a teaching hospital in Portland. They piloted the 4Ms at multiple sites, including MMC Hospital Elder Life Program (HELP) and MMC Geriatric Assessment Clinic, prior to moving to several inpatient units at MMC and the MMC emergency department.
One key lesson from this work was to identify and build champions. Champions “have the ability to share the data, share the stories, and share the impact,” said Peter Baker, LCSW, Program Manager of Geriatrics at MaineHealth. “I think that helps with that buy-in. And our champions have helped move us in different directions as well as to avoid missteps when we launch in new areas.”
Another lesson learned was to ensure that existing policies were being reliably implemented. For example, a policy was already in place to administer the Confusion Assessment Method (CAM) to assess for delirium. But from one PDSA cycle, the team learned that this was not consistently occurring. In response, they created a “badge buddy” — a wearable education tool with quick tips on delirium prevention and other information — and offered additional education. As a result, they were soon able to reestablish the CAM administration as a norm.
A third lesson was to include electronic health record (EHR) team members at the outset and involve them in work. “Chart reviews are always cumbersome and time-consuming. By involving the EHR team early we saved a lot of time,” Baker explained. This also helped collect “great data, which helped us measure the impact of our PDSA cycles moving forward,” he added.
While the 4Ms expansion was underway at the MMC inpatient sites, MaineHealth was also piloting the AFHS work in in their primary care practice and in a long-term care center, St. Joseph’s Rehabilitation Residence.
In these new settings, they drew on the insights from the MMC work. “We brought lessons learned, but we were also aware that when it comes to staffing, the EHR, and all sorts of other things, it’s a very different picture,” said Baker. For instance, long-term care settings still tend to engage in much more paperwork than computer work, which required adaptation.
There are also advantages to nursing homes. “One of the benefits in nursing homes is that people are there longer because it’s their home,” said Baker. “So, we can gather those stories, and learning what matters can really impact care significantly. Sharing that across the care team can have such a beneficial impact for both the quality of care as well as staff competence and confidence.”
MaineHealth also piloted age-friendly care in several primary care practices. They took advantage of an initiative to increase the number of Medicare AWVs by ensuring that the 4Ms were embedded in these visits. AWVs are “not the only place we’re going to be assessing for the 4Ms,” said Baker, “but it is a great place to assess for all of them.” They made some adaptations to their EHR, primarily around asking what matters, and built an AFHS primary care dashboard.
“Some of the lessons we’ve learned from the ambulatory site is that many of the 4Ms are being done already with many of the patients,” said Baker. They learned to take advantage of frameworks already in place, adding the 4Ms only when needed. “Focus on gaps,” Baker advised.
You may also be interested in:
Are We Inadvertently Contributing to Discrimination Against Older Adults?
