Why It Matters

Photo by Laurynas Mereckas | Unsplash
Age-Friendly Health Systems is an initiative of the Institute for Healthcare Improvement (IHI) and The John A. Hartford Foundation, in partnership with the American Hospital Association and the Catholic Health Association of the United States. More than 2,700 care locations since 2018 have been recognized as Age-Friendly Health Systems, including hospitals, primary care practices, convenient care clinics, and nursing homes.
For many health care organizations, providing excellent care for older patients has always been key. Consequently, some may wonder if getting involved in the Age-Friendly Health Systems initiative — whose goal is to improve care for all older adults across the US — should be a priority.
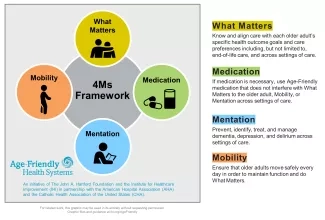
But taking part in the Age-Friendly Health Systems initiative has helped thousands of organizations across the country build on and expand the work they have been doing to provide optimal care for older adults. This has led to more than 1.4 million older adults receiving evidence-based care for older adults that reliably implements the “4Ms”: Asking What Matters to older adults, Medication, Mentation, and Mobility (see Figure 1).
Age-Friendly Health Systems convenes opportunities (called Action Communities) to provide guidance, offer support, and give participants chances to exchange ideas and best practices. In the following excerpts adapted from Age-Friendly Health Systems case studies on the University of Alabama Hospital and MaineHealth/Maine Medical Center, two Action Community organizations share what they have learned while implementing the Medication element of the 4Ms.
MaineHealth: Sleep Matters
MaineHealth, the largest health care organization in Maine, was already focused on improving care for older adults when their leaders saw the opportunity to get involved in Age-Friendly Health Systems. The initiative aligned perfectly with their goals, and in 2018, MaineHealth joined the Age-Friendly Health Systems Action Community.
For MaineHealth, the work started in a geriatrics program (The Hospital Elder Life Program) at Maine Medical Center. “We knew that we were doing a lot of the 4Ms already,” said Molly Anderson, Manager of Geriatrics Programs at Maine Medical Center. But the 4Ms framework helped them build on the work that was already underway. “In geriatrics we hear the 4Ms and we get it, and it makes a lot of sense to us,” said Anderson. “It’s a really great framework to be able to describe [the work] to other people.”
As part of their work on medications, one of MaineHealth’s major goals has been to minimize the prescription of sleep aids, which are considered risky for older adults. They instead encourage alternative, non-pharmacological approaches to help with sleep, such as guided relaxation, white noise machines, headphones, earplugs, and avoiding daytime naps. They also try to be sensitive to individual needs and preferences. “If somebody is a night owl,” said Anderson, “let them be a night owl.”
For Anderson, it all comes back to What Matters. The What Matters element of the 4Ms Framework focuses on knowing and aligning care with each older adult’s specific health outcome goals and care preferences. “What does this patient do at home when they can’t sleep? Some patients might like herbal tea, but for others that might keep them up all night using the bathroom,” Anderson said. Adjusting the timing of medication administration, so that it does not occur in the middle of the night, can also help.
As an example of how the 4Ms are mutually reinforcing, regular mobility during the day can help enormously with sleep. “As much and as safely as [older patients] can be up and moving, the better they’re going to sleep, the faster they can get out of the hospital,” Anderson noted.
In addition, a pharmacist worked with the cardiology and trauma teams to assemble two teaching modules: one on the risks of sleep aids and the other on the risks of polypharmacy. The pharmacist gave recorded presentations, which all the nurses and providers were assigned to watch.
If not for COVID-19, they probably would not have recorded the presentations; the fact that they did was a silver lining of the pandemic. Now these recordings are available for others to watch as well, which will be helpful as the age-friendly work spreads throughout the system. “This highlights the interdisciplinary approach we took to education around high-risk medications for older adults,” said Anderson. “The feedback from nursing is that they feel more confident in their communication with providers overnight to decrease use of higher-risk sleep aids.”
The University of Alabama Hospital: Collaboration is Key
The University of Alabama (UAB) Hospital, a teaching hospital that is the third largest public hospital in the US, launched its Acute Care for Elders (ACE) unit in 2008. In 2018, UAB leaders heard about Age-Friendly Health Systems and immediately knew they wanted to be involved. “We’d been working toward this goal of being age-friendly for a decade,” said Kellie Flood, MD, Associate Chief Medical and Quality Officer for Geriatrics and Care Transitions at UAB Hospital. “We were thrilled to get in the first Action Community cohort.”
For the Medication component of the 4Ms framework, the team started by creating flags for some of the high-risk medications for older adults, such as antihistamines and sedatives. In the electronic health record, they introduced pop-up flags for patients ages 65 and older that not only provide warnings, but also suggest safer alternatives, making the alerts more useful.
The ACE unit holds a daily team meeting that includes a pharmacist. Together, the team scans the medication list for every older adult, looking for opportunities to prescribe lower doses or to discontinue a medication altogether. Flood and the team expanded on this work by partnering with the hospital’s surgical services. For example, they worked with orthopedic surgeons on an orthopedic surgery order set for older adults, identifying high-risk medications and considering alternatives. Most recently, they worked with urogynecology and gynecology surgeons to adjust their order sets.
“Partnering with our surgeons has been one of the highlights of our age-friendly journey. It’s such a win-win for everyone, especially the patients,” said Flood. “I think the key [to the partnership] is we don’t go in and tell a group of GI surgeons or orthopedic surgeons what to do,” Flood continued. “We’re all working toward the same goal, so we develop the age-friendly improvement strategies together.”
The UAB team has seen a decrease in the percentage of older adult patients with AGS Beers Criteria medications (i.e., potentially inappropriate medications for the elderly) ordered and administered from partnering surgical services. For example, the urogynecology and gynecology-oncology services saw a significant reduction in medications on the Beers Criteria list, from 38 percent to 12 percent.
Flood noted that, like all improvement work, making care more age-friendly is a continuous process. “You always have to be on the lookout, double-checking that the processes you put in place are still in place.” She added, “This is a lifelong journey, but it’s also fun and rewarding. Be sure and celebrate your team and their successes along the way.”
One of those successes was evident on a day when Flood was the geriatrician on duty on the ACE unit, doing her charting in the same room as the “move and groove” session. “I was so uplifted by the music. I always find myself singing along,” she recalled. Then suddenly she saw a younger woman, the daughter of one of the older adults, start to tear up. Flood went over to her and said, “Are you OK?” The daughter explained that her mother had just come from another hospital and had been downcast, uncommunicative, and barely mobile. Now she was dancing. She told Flood, “You guys have given me my mother back.”
You may also be interested in:
