Why It Matters

I started using telemedicine around 13 years ago as a geriatrician for the US Department of Veterans Affairs (VA). I used it mostly for following up with patients after discharge from a Geriatric Evaluation and Management (GEM) Unit, which served as a longer-term rehabilitation unit that we had in our hospital.
I’ve seen how the VA has used telemedicine over the years, using numerous different platforms. They’ve used encrypted telephones that involved calling from a central location in a medical facility and video chat that required placement of equipment during a home visit.
We’ve run the gamut from using basic landline telephones to HIPAA-secure video-conferencing programs. These days, we sometimes place tablets in the home when the patient does not have access to a smartphone.
As more primary care is being shifted away from office visits during the COVID-19 pandemic, I’m now using my telemedicine experience and training as a geriatrician to help the VA use the 4Ms Framework for Age-Friendly Care to improve care for older adults.
The Advantages of Telemedicine
Given the need to prevent unnecessary exposure to the coronavirus, most patients don’t question why we’re shifting to telemedicine, but they still need help understanding that telemedicine can be an effective way to communicate with their providers. You never want them to feel that they’re not getting high-quality care.
The great thing about telemedicine is that you can schedule the visits to fits the patient’s needs. If they say, “I do best right around 1:00 PM,” you can make sure you’re calling at 1:00 when they’re at the peak of their energy. Televisits are especially good for frail, older people because they don’t get worn out from the traveling to your office.
In fact, if you think about any patient who lives in a rural area or takes public transportation to get to their doctor’s office, a televisit saves them from spending their whole day just going for an appointment. In those situations, a patient could easily spend hours traveling to the doctor’s office, having a 20- to 30-minute-visit, and then going back home. That is not the best use of anyone’s time or energy.
An Easy Way to Make Telemedicine Age-Friendly
One of the things that providers often find challenging during televisits is addressing everything they want to cover without sounding like they’re checking boxes off on a list. Patients don’t appreciate feeling like the interaction is impersonal or that their provider is just going through the motions. For this reason, the 4Ms (see Figure 1) is fantastically helpful for guiding a televisit.
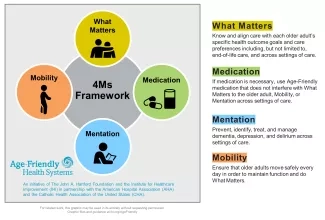
While helping with the telemedicine conversion in the clinics for our local VA, I recommend providers — many of whom are feeling overwhelmed by suddenly having to make this change — use the 4Ms Framework as a reliable and useful script to follow:
- What Matters — Asking patients about their goals, preferences, and priorities is a great way to build rapport at the start of a telemedicine visit and ensure that it’s person-centered. Right now, many people may prioritize avoiding COVID-19. Their provider can build a care plan around reinforcing physical distancing and making sure they have all their basic needs met. How are you getting food? Do you have help from your family? If not, what resources are in your community? Are you a member of a religious organization? Do you belong to a club? We can encourage patients to reach out to people they know who might be willing to help with things like getting groceries delivered.
- Medication — Using a shared understanding of what matters most to the person, a provider might then ask to see the medications the patient is taking. Do you understand how and why you’re taking these medications? Does any medication you’re taking get in the way of achieving what matters most to you? We want to deprescribe medications they no longer need, but during this COVID-19 crisis, we also need to make sure they have an adequate supply of their medications. We don’t want them to take half the correct dose because they’re afraid of running out, for example.
- Mentation — It’s essential to address a patient’s cognition during every televisit. It doesn’t have to be extensive, but a brief screening to assess cognitive impairment will help make sure the discussion you’re having will be remembered or understood. What day of the week is it? Can you list the months of the year backwards, starting with December?
- Mobility — The great thing about addressing mobility during a televisit is you can see how the person gets around in their own home. Ask them to get up out of their chair and walk a few steps. While people are practicing physical distancing, you can discuss plans to stay active while at home. They can do laps around a room or around a house. You can advise them to do five to 10 sit-to-stand repetitions three to four times a day.
Laurence M. Solberg, MD, is a geriatrician with the US Department of Veterans Affairs.
You may also be interested in:
