Why It Matters
Respectful end-of-life care is concordant with patients’ stated goals, values, and preferences —in other words, honoring what matters most to them at the end of life. Goal-concordant care is pursued through the process of advance care planning (ACP), which strives to both ensure that patients (or their surrogate medical decision makers) understand their diagnosis, prognosis, and treatment options, and health care professionals understand what matters most to their patients.
The failure to respect patients’ wishes regarding end-of-life care can lead to harm — including emotional, psychological, socio-behavioral, and financial harm — meaning that poor end-of-life care is a safety issue.
Assessing whether end-of-life care has been respectful is challenging, but critical. The following excerpt from IHI’s “Conversation Ready”: A Framework for Improving End-of-Life Care (Second Edition) white paper describes the Respect Measurement Tool in Appendix B. While the tool requires more development and testing, it has demonstrated promise and may promote more productive conversations between care teams and families about the patient’s experience.
While IHI and other organizations are still learning about this area of work, we have found it useful to measure respect from the perspectives of patients and families and health care professionals.
Patient and Family Perspective
Measuring respect requires asking patients about what respectful care means to them. For patients who have lost the capacity to speak for themselves or who have died, it is reasonable to ask their family or other surrogate medical decision maker (although it may be difficult to determine whether they know enough to answer accurately on behalf of the patient).
Accordingly, consider several approaches:
- Conversations with patients and families, including those living with serious illness, for instance, this resource from Healthcare Improvement Scotland: Person-Centred Health and Care: Real-time and Right-time evaluation report
- Measures of shared decision making, for instance, the collaboRATE™ instrument that asks patients (or families) to rate their answers to three simple questions (e.g., using a 1-to-5 rating scale):
- How much effort was made to help you understand your health issues?
- How much effort was made to listen to the things that matter most to you about your health issues?
- How much effort was made to include what matters most to you in choosing what to do next?
- Post-mortem surveys or conversations with families, for instance, the National Hospice and Palliative Care Organization’s Family Evaluation of Hospice Care, which includes the following questions:
- At any time while the patient was receiving palliative care, did the doctor or another member of the medical care team do anything with respect to end-of-life care that was inconsistent with the patient’s previously stated wishes?
- While the patient was receiving palliative care, how often did the medical care team treat him/her with respect?
- While the patient was receiving palliative care, how well did the medical care team do at providing care that respected his/her wishes?
Health Care Professionals Perspective
Teams can use the tool as a basis for reflection and conversation about their provision of respectful care. The tool provides a structured way to conduct inquiry — allowing teams to consider care from multiple dimensions and surface opportunities to improve. In addition, teams might track the total scores over time as a rough indicator of overall provision of respectful care.
While still in the early stages of testing, the tool is intended to help organizations quickly understand and learn about how well they are respecting patients’ wishes at the end of life and prompt valuable conversations with patients, family members, and health care professionals.
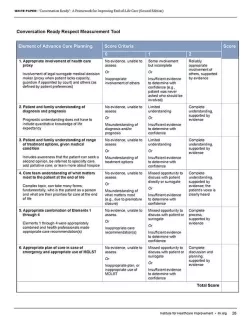
Asking professionals to reflect on whether they are providing respectful care may be a powerful, if limited, way to drive improvement. The Conversation Ready Respect Measurement Tool (see below) asks health care professionals to score the degree to which six key elements of advance care planning were addressed with a given patient.
Organizations can use the Respect Measurement Tool retrospectively (to review records of patients who have died, to identify and understand system-level problems and focus future improvement work) and prospectively (to identify care gaps with patients who are still alive and provide more respectful care while there is still time to do so).
To learn more about how to measure your organization's readiness to reliably receive, record, and respect patients’ end-of-life care wishes, download the free IHI “Conversation Ready”: A Framework for Improving End-of-Life Care (Second Edition) white paper.
You may also be interested in:
