Why It Matters

Can you rebuild trust when trust is absent? Can you strengthen trust when it is not just weakened but broken?
These are two of the provocative questions recently asked by the Institute for Healthcare Improvement (IHI) Innovation Team. The Innovation Team serves as IHI’s internal engine for research and development of new care models. We explore promising improvement ideas in health care that may not yet have received the attention they deserve.
In partnership with the American Board of Internal Medicine Foundation (ABIMF) the Innovation Team chose to focus on the issue of trust because it links to work IHI has done on joy in work and workforce well-being, equity, and psychological safety. IHI President and CEO Kedar Mate also addressed trust in his 2021 IHI Forum keynote. Most importantly, while some communities and individuals described a lack of trust in health systems well before COVID-19, we decided it was important to address how the strain of the health crisis has further undermined trust in a variety of ways for both the public and the health care workforce.
Learn more about IHI's Innovation work at the IHI Forum
The ABIMF has done work on trust between individual patients and providers, so IHI decided to build on that by bringing our expertise in looking at systems to explore organizational trust. While it is common to focus on the interpersonal aspects of trust in health care, it became clear in our research that systems can act in ways to either build or erode trust. Particularly when thinking about communities, trust is more than just how you interact with your individual doctor. The culture of a health system and how people within it interact with communities is systemic and not strictly interpersonal. We decided it would be important to highlight these issues and offer guidance on how best to leverage ways to build trust at the system level.
Incorrect Assumptions of Trust
The original idea for IHI’s collaboration with the ABIMF was to research opportunities to strengthen trust. Due in large part to interviews my Innovation Team colleague, Bhargavi Sampath, did with community members and health systems, we found that many organizations have a trust deficit because of the historical and current harms that marginalized groups and especially BIPOC people experience. The research made it clear that health care systems cannot focus solely on strengthening trust because that assumes that trust already exists.
These kinds of assumptions ignore the institution’s own history and the history of how medicine has too often been practiced in the United States. In other words, before you can build or strengthen trust, you must first acknowledge and address the wrongs that have been done. These wrongs may have happened under someone else’s leadership, but they still need to be addressed before you can build real trust.
For example, during our research we found an organization that recognized they had a painful legacy both internally and externally to overcome. They acknowledged that there were Black staff members in their 60s whose mothers were not allowed to give birth in their maternity ward. This was a big part of why the community did not have longstanding positive connections with this hospital. They are now trying to understand if they can develop a process or space for building those relationships.
Trust Between Clinicians and their Organizations
Another aspect of our research was exploring the clinician experience of trust. A lot of the research in our initial review of the literature indicated that the biggest influences on a clinician’s experience of trust were their managers and the people immediately above them in the institutional hierarchy. We then had a pivotal interview with Mark Linzer, MD, a physician and the Director of the Hennepin Healthcare Institute for Professional Worklife and IHI joy in work and workforce well-being faculty member. He asks some key questions to understand the systemic influences on clinician well-being: Are clinicians allowed to work at the top of their license? Are clinicians in the room when organizations make high-level decisions that are going to affect them, their patients, or how they are allowed to practice? Are they able to exert some control over their workday in a way that provides them joy in work and well-being and gives them a sense of autonomy?
Many of the factors influencing joy in work and workforce well-being were similar to what promotes trust with communities. Are you co-designing with communities or are you just telling them what you think they should do? Are you tapping into the knowledge of the community you have within your own organization throughout your workforce? Who decides on the organization’s stated values? Is it just a few people sitting in a room? Or is every level of your staff choosing — and not just commenting on — those values?
Clinicians want to provide high-quality care for their patients, but they sometimes feel that many of the things preventing them from doing the best for their patients are top-down, systemic decisions. For clinicians, building or strengthening trust means seeking values alignment between the workforce and the leadership. How can we make those values and those misalignments explicit? How do we hold each other accountable so decisions being made are in pursuit of those values? The misalignment of values between the C-suite and what clinicians are doing on the ground breeds distrust in the system.
Keys to Rebuilding or Strengthening Trust
To offer a blueprint for rebuilding or strengthening trust, we adapted a framework known as the Healing ARC developed by Michelle Morse, MD, MPH, and Bram Wispelwey, MD, MPH, of Brigham and Women's Hospital in Boston.
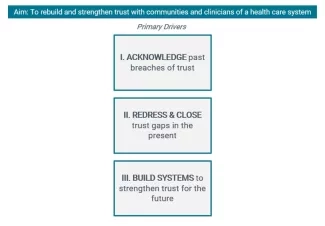
In our three-step model, there are three keys to rebuilding and strengthening trust:
- Acknowledge what has happened before and take ownership and responsibility.
- Take steps to redress harm and course correct to close current gaps in trust in ways that are agreed upon by the community or the clinician. This means more than a health care system deciding on their own to show up to an event or offering resources that no one requested. This means asking communities what they need and want. This means responding in a way that is in line with the values and needs of those harmed.
- Once you have taken steps one and two and you are in a process of building a foundation of trust, ask what you can do to strengthen and cement the trust. This may mean being more embedded in the community, allowing yourself to be held accountable by the community, and investing in the community, particularly around equity. The key is determining how a health care organization can use its power to invest in and encourage ways for the community to benefit from using its own assets. How can a hospital use an asset-based — rather than deficit-based — perspective and help build upon the momentum, energy, resources, will, and organizing that already exists in the community?
During our research, a lot of people told us that trust can be hard to define, but you know what it is when you experience it, and you also know when it is gone or is not there. Understanding the meaning of trust and how to build or strengthen it has always been important for any health care organization, but many experiences exacerbated or created by the COVID-19 pandemic – from vaccine hesitancy to workforce shortages – have now made this essential.
Keziah Imbeah, MSc, is a Senior Research Associate on the IHI Innovation Team.
You may also be interested in:
What I Am Learning About Trust
It’s Not You, It’s Us: Earning Trust to Build Community Connections
The IHI Innovation System white paper
