Summary
- We miss a crucial piece of the patient safety puzzle when we do not incorporate an equity lens when analyzing adverse events.

Event analysis is a valuable tool to improve patient safety and quality of care by identifying root causes of incidents and implementing corrective actions to prevent future similar events from occurring. When we analyze adverse events in health care and do not incorporate an equity lens, however, we are missing a crucial piece of the investigative puzzle.
Health equity is essential to improving health and well-being and can be costly if not addressed. Studies have shown that bias and inequities can contribute to patient safety events. Examples include:
- “Asian and Hispanic patients hospitalized with acute cardiovascular disease, pneumonia, and major surgery had significantly higher rates of hospital-acquired infections when compared to white non-Hispanic patients.”
- “49.1 percent of limited English proficient patient adverse events involved some physical harm whereas only 29.5 percent of adverse events for patients who speak English resulted in physical harm.”
- “At safety net hospitals, homeless adults hospitalized for acute myocardial infarction were less likely to receive coronary angiogram, percutaneous coronary intervention, and coronary artery bypass graft compared with non-homeless adults.”
Ignoring bias and inequities leads to incomplete corrective action plans that fail to address all root causes of an event. While there is standard guidance on how to conduct event analysis, guidance regarding consideration of bias and inequities is limited. We describe an approach at NYC Health + Hospitals, the largest municipal health system in the United States, on how to embed equity into every step of event analysis.
Challenges Embedding Equity in Event Analysis
To begin, we asked frontline staff and leadership for feedback to identify challenges (Figure 1). We concluded that many of the challenges fall under three main categories: knowledge and comfortability, data methodology, and leadership support. We wanted to ensure these categories were addressed in all stages of event analysis.
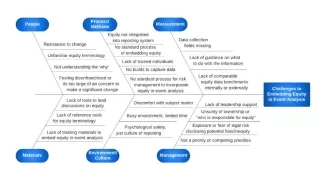
Figure 1. Fishbone of challenges to embedding equity in event analysis. Source: NYC Health + Hospitals
The major steps of event analysis include the reporting of the event through the event reporting system, the investigation of the event, and if applicable, root cause analysis (RCA) and corrective action planning. Using the three major themes of knowledge and comfort, data methodology, and leadership support, we suggest specific interventions at each stage of event analysis.
We recognize that event analysis is often reactive, focusing on improvement after an event has occurred. Therefore, alongside equitable event analysis, we suggest creation and implementation of a proactive training and reference tools specifically focusing on preventing equitable care issues and reducing bias in patient safety for all staff.
Event Reporting
- Knowledge & comfort: Training and standard tool for identification of bias with everyday examples of bias in patient safety events.
- Data methodology: Embed mandatory fields for demographic and social determinants. information into the event reporting system and embed a mandatory question into the event reporting system: “Did bias or equitable care issues potentially contribute to this event?”
- Leadership support: Leaders encourage staff to report events and build psychological safety and recognition for reporting.
Investigation
- Knowledge & comfort: Training for investigators on identification of bias and equitable care issues, including how to interview staff with a focus on equity.
- Data methodology: Ensure equity data fields are built into the electronic medical record for easy identification for the RCA write-up.
- Leadership support: Risk management and patient safety leadership set expectations that an equity lens be included in the investigation process.
Root Cause Analysis
- Knowledge & comfort: Use standard tools for identification of bias and equitable care issues discussed during the RCAs. Share evidence of existing equitable care issues for the adverse event either in literature or past data.
- Data methodology: Integrate social determinants of health data into the RCA standard form. Incorporate a bias section into fishbone diagram.
- Leadership support: Executive leadership ensures time is set aside in the RCA for an equity discussion and helps facilitate the discussion, Incorporate equity discussion of adverse events in dialogue with the highest levels of leadership.
Corrective Action Planning
- Knowledge & comfort: Provide training on types of interventions that reduce inequities.
- Data methodology: Investigate historical data on inequities with other similar adverse events. Set an aim statement to reduce bias/focus on equitable care issues in the current event and track data over time.
- Leadership support: Regularly report on corrective action progress with an equity lens in departmental and hospital-wide meetings.
An Opportunity to Close the Gap
After receiving training on how to ingrain equity into event analysis, one of our patient safety leaders stated that they have a much better understanding of how to craft more robust corrective action plans that address structural bias and injustice. Since participating in training, they have found opportunities during root cause analysis to address equitable care opportunities such as increasing availability of devices for interpreter services and developing standardized workflows for evaluation of abdominal pain in female patients.
As a community, we have an opportunity to advance equitable health care by including equity in event analysis and throughout patient safety work. This serves as a call to action to prioritize health equity in every step of event analysis. This includes developing comprehensive corrective action plans that create a culture of equity and lead to better outcomes for all.
Komal Chandra, PhD, MMH (@KomalChandraPhD), is the Director of Operations, Patient Safety and High Value Care at New York City Health + Hospitals. Mariely Garcia, BA, is a medical school student at ICAHN School of Medicine. Komal Bajaj, MD, MS-HPEd (@KomalBajajMD), is the Chief Quality Officer at NYC Health + Hospitals/Jacobi/North Central Bronx. Janette Baxter, RN, MS, Esq, is the Assistant Vice President Risk Management & Continuing Professional Education, at New York City Health + Hospitals. Regina Wallace, JD, RT, is the Director of Risk Management at New York City Health + Hospitals. Hillary Jalon, MS, is the Vice President Quality Management at New York City Health + Hospitals. Eric K. Wei, MD, MBA, is the Chief Quality Officer at New York City Health + Hospitals. Mona Krouss, MD, FACP, CPPS (@KroussMD), is the Assistant Vice President of Value and Patient Safety at New York City Health + Hospitals.