Why It Matters
With a mission to serve poor and vulnerable people, Providence, a large health system with locations in seven states in the American West, is committed to moving beyond “Health 1.0.” According to Jennifer Bayersdorfer, MHA, Senior Vice President & Chief Quality Officer, Health 1.0 is defined as “invest[ing] our dollars in hiring specialists who are driving dollars to our hospitals.”
Instead, Providence sees the path to the future as “Health 2.0,” which they call “Destination Health.” This new model is centered around patients and their families, and instead of being hospital-oriented, the care meets patients where they live, work and play.
“Older adults, especially frail elders, are among the most vulnerable in our communities,” said Bayersdorfer, and as part of its commitment to serving this population, Providence was one of five pioneers who first participated in Age-Friendly Health Systems (AFHS) in 2017. AFHS is an initiative of the Institute for Healthcare Improvement (IHI) and The John A. Hartford Foundation, in partnership with the American Hospital Association and the Catholic Health Association of the United States. In Age-Friendly Health Systems, age-friendly care is defined as care that is based in the “4Ms”: What Matters, Medication, Mentation, and Mobility (see Figure 1).
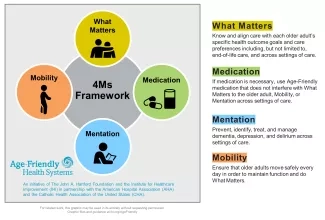
As a pioneer, Providence was involved in testing and refining the 4Ms. They also, based on identified needs in their patient population, added a 5th M: Malnutrition. And since then, they have been working to scale up the 4Ms + Malnutrition throughout the system.
Bayersdorfer leads the age-friendly effort at Providence, acting as the hub for coordination. She and her colleagues have been working to innovate and transform the care they provide. “We need to be looking at not just people who need a hospital but people who need care,” said Bayersdorfer. “And how can we care for, in this case, an older adult population in a way that focuses in on what matters most to them?”
Bayersdorfer and her colleagues think of 4Ms + Malnutrition care “as a bundle of interventions that we want to deliver to every patient every time in every setting.” That includes specialty care. “How are we within neurosciences or cardiovascular or digestive health ensuring that we’re reflecting the [4Ms + Malnutrition] care even in the specialty experiences that we’re delivering?”
To scale the 4Ms + Malnutrition within the system, they have taken several approaches. They have launched their own age-friendly action community, recruiting teams that will work on plan-do-study-act cycles (PDSAs) to drive 4Ms + Malnutrition care. They’re also building the 4Ms + Malnutrition into what they call “Caring Reliably Commitments,” which refers to the components of care they want to see consistently throughout the system.
Providence takes a “tight/loose/tight” approach to scale. “We are clear around the why and the what we’re trying to accomplish, and how we’ll measure it,” explains Bayersdorfer, “but we are loose in terms of how it gets implemented, so it can be supported by the unique resources and teams at each of our settings.”
They also conduct research to advance healthy aging. In 2021, they launched an innovation challenge for new ideas related to basic 4Ms + Malnutrition innovation. One of their awards went to their geriatric nurse practitioner programs to reformulate their curriculum to center around the 4Ms + Malnutrition.
In terms of measurement, for overall outcome, they’re looking at Medicare spending per beneficiary, risk-adjusted mortality, and readmission rates. They also have robust measurement around goals of care conversations. For Mentation, they deploy a number of screening tools that help them to determine when patients are experiencing depression or dementia. Their overall goal is to build assessments into routine care and use the results to connect patients with appropriate follow-up care.
Providence also has a geriatric mini-fellowship for primary care providers that is focused on a 4Ms curriculum. Participating providers then go back to their clinics and work on integrating the 4Ms into Annual Medicare Wellness visits and other aspects of their practice.
Bayersdorfer has found that the 4Ms + Malnutrition offer providers a means to simplify and streamline their care. This “eases their way and allows them to feel a sense of confidence, competence and care in what they’re doing.” That, in turn, helps Providence to continually improve care “and keep serving the communities we care so much about.”
You may also be interested in:
How Even the Best Geriatric Care Can Get Better
Using the Age-Friendly 4Ms to Better Advocate for Older Adults (and Geriatric Care)