شراكة متعددة السنوات بين IHI ومؤسسة سانت جود العالمية لنشر أفضل الممارسات لإدارة مرضى سرطان الأطفال الذين يراجعون قسم الطوارئ مصابين بالحمى
تعاونيات "الساعة الذهبية" - دقائق تنقذ الأرواح
نظرة سريعة على التأثير: تعاونات "الساعة الذهبية"
60%
increase in patients receiving the first dose of antibiotics within 60 minutes
60%
decrease in incidence of sepsis
27
deaths avoided
$8-10
million in avoided costs
Paola Friedrich, MD
Mexico and Central and South America Regional Programs Director St. Jude Global
Mexico and Central and South America Regional Programs Director St. Jude Global
“We know the Golden Hour works. Now we have robust data to show it works in diverse real-world settings across Latin America and that, working together, health care teams and institutions can reduce preventable sources of morbidity and mortality, reduce unwanted variations in care, anchor service delivery on the patient and their experience and improve the overall quality of care being delivered.”
ملخص
تُعدّ العدوى السبب الأول للوفاة بين الأطفال المصابين بالسرطان. وقد أثبتت "الساعة الذهبية" - إعطاء المضادات الحيوية خلال ساعة - فعاليتها في الحد من العدوى والمضاعفات المرتبطة بها والوفيات لدى مرضى الأورام الدموية لدى الأطفال المصابين بالحمى (PHOPf) الذين يراجعون قسم الطوارئ. منذ عام ٢٠١٩، يتعاون معهد تحسين الرعاية الصحية ( IHI) ومؤسسة سانت جود العالمية لنشر "الساعة الذهبية" بفعالية في جميع أنحاء أمريكا اللاتينية من خلال برنامجين تعاونيين لتحسين الجودة (QICs) وبرنامجين لعلم التحسين العملي (ISIA)، بهدف زيادة نسبة مرضى الأورام الدموية لدى الأطفال المصابين بالحمى (PHOPf) الذين يتلقون الجرعة الأولى من المضادات الحيوية خلال "الساعة الذهبية" إلى ٧٠٪.
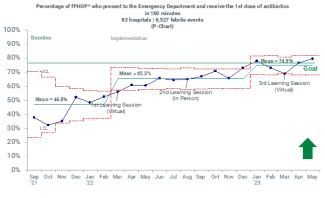
استخدمت مراكز تحسين الجودة نموذجًا Breakthrough Series Collaborative، إلى جانب تدريب على تحسين الجودة. عُقدت أول دورة من دورات تحسين الجودة بين مايو 2019 ونوفمبر 2020، وشارك فيها 23 مستشفى من المكسيك. أما الدورة الثانية، فقد عُقدت بين نوفمبر 2021 ومايو 2023، وشارك فيها 85 مستشفى من المكسيك وأمريكا الوسطى والجنوبية.
لقد تجاوزت مشاريع التعاون التابعة لـ MAS أهدافها (انظر النتائج المحددة أدناه) وفي الوقت نفسه أنشأت شبكة دائمة ومتعددة الجنسيات من الأطباء المدربين على تحسين الجودة - وهو مورد لا يقدر بثمن للتحسينات المستقبلية.
- زيادة بنسبة 60% في عدد المرضى الذين يتلقون الجرعة الأولى من المضادات الحيوية خلال 60 دقيقة
- انخفاض بنسبة 60% في حالات الإنتان
- تم منع ما يقدر بنحو 347 حالة من حالات الإنتان
- تم تجنب ما يقدر بنحو 27 حالة وفاة
- تم تخفيض ما يقدر بـ 5458 يومًا من أيام الإقامة في المستشفى
- على الأقل (ما يقدر بنحو) 8-10 ملايين دولار من التكاليف المتجنبة
خلفية
يُصاب ثلث مرضى الأطفال الذين يخضعون للعلاج الكيميائي بنقص العدلات الحموي. في البلدان منخفضة ومتوسطة الدخل، تتراوح نسبة الوفيات المرتبطة بالعلاج والمرتبطة بالمضاعفات المعدية بين 10% و25%؛ بينما تقل عن 2% في البلدان مرتفعة الدخل. ونظرًا لأن العدوى تُشكل مخاطر كبيرة على الأطفال الذين يتلقون علاج السرطان، فإن أفضل الممارسات القائمة على الأدلة هي إعطاء المضادات الحيوية خلال 60 دقيقة من فرز الحالات. تُعرف هذه الفترة الزمنية باسم "الساعة الذهبية" نظرًا لفعاليتها في الحد من المضاعفات والوفيات المرتبطة بالعدوى.
بين عامي 2016 و2019، وفي إطار جهودها لنشر أفضل الممارسات، أطلقت سانت جود العالمية وبرنامجها الإقليمي في المكسيك برامج تجريبية لتحسين الجودة تهدف إلى ضمان تطبيق هذه الممارسة في تيخوانا وكولياكان وغوادالاخارا. في عام 2019، أطلق البرنامج الإقليمي في المكسيك أول برنامج تعاوني "الساعة الذهبية" في المكسيك بالتعاون مع Institute for Healthcare Improvement. وقد أشرك هذا البرنامج التعاوني 23 مستشفى في المكسيك، وزاد نسبة مرضى أمراض الدم والأورام لدى الأطفال المصابين بالحمى الذين يتلقون الجرعة الأولى من المضادات الحيوية من متوسط أساسي بلغ 40% إلى 78% في جميع المواقع المشاركة على مدار 18 شهرًا.
لقد أدى نجاح هذا التعاون الأول لـ MAS إلى مبادرة موسعة - التعاون الثاني لـ MAS.
يقترب
التعاونيات هي برامج تحسين جودة تعتمد على نموذج Breakthrough Series التابع لمعهد تحسين الرعاية الصحية (IHI )، وهو نهج طورته IHI في تسعينيات القرن الماضي بهيكلية بسيطة لكنها فعّالة تُسهّل التحسين على مستوى مجموعة كبيرة من الفرق المشاركة. الهدف من جميع التعاونيات في Breakthrough Series هو سد الفجوة بين ما نعرفه من نجاح وما نفعله فعليًا في مجال الرعاية الصحية.
وقد اتبع المشروع التعاوني الثاني لـMAS، مثل المشروع الأول، نموذج BTS، وكان بمثابة آلية لتوسيع نطاق الساعة الذهبية إلى 72 مستشفى في المكسيك و13 مستشفى في خمس دول إضافية في أمريكا اللاتينية.
يتألف نموذج BTS من خمسة عناصر أساسية: 1) التركيز على موضوع محدد ومشترك؛ 2) الدعم المستمر من خبراء تحسين الجودة وخبراء المجال؛ 3) مشاركة فرق من مواقع أو منظمات متعددة؛ 4) استخدام نظرية مشتركة للتغيير واستراتيجية قياس؛ 5) استخدام Model for Improvement (MFI) كإطار توجيهي له. وقد اقترن نموذج BTS ببرنامجين تدريبيين لتحسين الجودة لبناء القدرات والكفاءات المحلية في مجال تحسين الجودة، سعياً لتعزيز الجودة داخل المؤسسات المشاركة وضمان الاستدامة.
نُظِّمت تعاونات MAS على شكل جلسات تعلم حضورية وافتراضية وفترات عمل. خلال فترات العمل، اختبرت الفرق أفكار التغيير باستخدام دورات Plan-Do-Study-Act (PDSA) القائمة على نظرية مشتركة للتغيير؛ وحضرت مكالمات تعليمية شهرية؛ وتلقت تدريبًا؛ وأبلغت عن دورات التخطيط والتنفيذ والدراسة والتنفيذ والبيانات في مستودع مشترك.
ساعد نموذج BTS في تمكين التوسع بشكل كبير من 23 موقعًا أوليًا في المكسيك إلى 72 مستشفى في المكسيك و13 مستشفى منتشرة في جميع أنحاء البرازيل وهايتي وبنما وباراغواي وبيرو.
عمل فريق البرنامج مع المشاركين لاختبار وتحسين نظرية التغيير المُفصّلة في مخطط العوامل المُحفّزة ، وهي أداةٌ شائعة الاستخدام من قِبل IHI) لربط الهدف العام للبرنامج بأفكار تغيير مُحدّدة لاختبارها. في ورشة العمل التعاونية الثانية "الساعة الذهبية"، نظّمت الفرق أفكار التغيير واختبرتها وفقًا للعوامل الرئيسية التالية: 1) الوصول إلى المستلزمات والأدوية وتوافرها؛ 2) نظام فعّال لإدارة البيانات والتعلّم؛ 3) تعزيز الكشف المُبكر عن الحمى في المنزل وتوفير الرعاية في الوقت المُناسب؛ 4) زيادة موثوقية العمليات السريرية؛ 5) تعزيز العمل الجماعي والتواصل الفعال.
جمع نظام التعلم بيانات كمية ونوعية مُنتَجة من خلال المقابلات ومجموعات التركيز. واستخدموا هذه البيانات لتقييم أثر التغييرات، وإعادة تصميمها، واستكشاف تغييرات جديدة ذات إمكانات.
نتائج
بالإضافة إلى النتائج المذكورة أدناه، ساهمت المشاركة في برامج التعاون مع MAS في بناء القدرات المحلية في أساليب وأدوات التحسين. وأصبح بإمكان الفرق المشاركة الآن إطلاق مشاريع وبرامج جديدة لتحسين الجودة، وجمع وتحليل البيانات اللازمة لتقييم الأثر وتوجيه المبادرات المستقبلية.
كما شكّلت تعاونيات MAS شبكة إقليمية راسخة من الأطباء من مختلف البلدان، ممن عملوا معًا لنشر وتطبيق أفضل الممارسات المُجرّبة. هذه المزايا الإضافية ليست وليدة الصدفة، بل هي النتيجة المرجوّة لنهج IHI في التحسين التعاوني.
حقق التعاون الثاني لـMAS أهدافه وأنتج النتائج التالية:
- زيادة بنسبة 60% في عدد المرضى الذين يتلقون الجرعة الأولى من المضادات الحيوية خلال 60 دقيقة (انظر الرسم البياني أدناه)
- انخفاض بنسبة 60% في حالات الإنتان
- تم منع ما يقدر بنحو 347 حالة من حالات الإنتان
- تم تجنب ما يقدر بنحو 27 حالة وفاة
- تم تخفيض ما يقدر بـ 5458 يومًا من أيام الإقامة في المستشفى
- على الأقل (ما يقدر بنحو) 8-10 ملايين دولار من التكاليف المتجنبة