Age-Friendly Health Systems
According to the US Census Bureau, the US population aged 65+ years is expected to nearly double over the next 30 years, from 43.1 million in 2012 to an estimated 83.7 million in 2050. These demographic advances, however extraordinary, have left our health systems behind as they struggle to reliably provide evidence-based care to every older adult at every care interaction.
What Is an Age-Friendly Health System?
Age-Friendly Health Systems is an initiative of The John A. Hartford Foundation and the Institute for Healthcare Improvement (IHI), in partnership with the American Hospital Association (AHA) and the Catholic Health Association of the United States (CHA), designed to meet this challenge head on.
Age-Friendly Health Systems aim to:
- Follow an essential set of evidence-based practices;
- Cause no harm; and
- Align with What Matters to the older adult and their family caregivers.
Learn more about upcoming Action Communities and the new Online Course with Coaching
What Does It Mean to Be an Age-Friendly Health System?
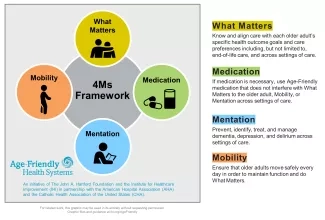
Becoming an Age-Friendly Health System entails reliably providing a set of four evidence-based elements of high-quality care, known as the “4Ms,” to all older adults in your system: What Matters, Medication, Mentation, and Mobility.
4Ms Framework of an Age-Friendly Health System
Learn more about How to Practice the 4Ms by Care Setting

Join the Age-Friendly Health Systems Movement
Action Communities
Age-Friendly Health Systems Action Communities enable teams to accelerate reliable practice of the 4Ms in an active community of learners and testers.
Online Course with Coaching
The Age-Friendly Health Systems Online Course with Coaching teaches the elements of the 4Ms Framework and develops your ability to provide age-friendly care in various care settings.
Getting Started Guides
Numerous guides and other resources are available to support your Age-Friendly Health System journey.
Recognition
Become recognized as an Age-Friendly Health System.
Why Become an Age-Friendly Health System?
Connect and Learn with the Age-Friendly Health Systems Movement
Join Friends of Age-Friendly Health Systems for updates about the movement, notification about quarterly webinars, access to experts, and further support on the 4Ms Framework.
- Sign up for the Friends of Age-Friendly newsletter
- Friends of Age-Friendly Webinars: Recording links and descriptions for each webinar
Upcoming Webinar: Join the Friends of Age-Friendly webinar on Thursday, February 5, 2026 at 3 PM ET to hear about the Age-Friendly Health Systems movement. Presenters include the IHI team, The John A. Hartford Foundation, Veterans Health Administration, and Hudson Hospital! Learn about our team, movement updates, new resources, and more! If you have any questions, please reach out to AFHS@ihi.org. Below is the information to join our virtual webinar.
- Zoom Link
- Meeting ID: 853 1405 8958
- Passcode: Friends26!
Join Friends of Age-Friendly Health Systems
Receive updates on the Age-Friendly Health Systems movement, invites to quarterly webinars, access to experts, support on the 4Ms Framework, and more.
Join the Community
