Why It Matters
Inspired by the work of NYC Health + Hospitals' efforts to embed health equity into their adverse event analysis, WellSpan Health shares their self-assessment so others might likewise learn from their efforts.
Depending upon the structure of one’s organization, it can be easy to treat health equity as separate from work to improve quality of care. If, however, your own data is telling you that there are quality gaps when you stratify it by race, such inequities are impossible to unsee. Whether the numbers indicate a higher mortality rate among Black patients or a disproportionate incidence of chronic illness among people of color, dedicated quality improvers have an obligation to ensure that their efforts truly improve care for all.
A few months ago, the Institute for Healthcare Improvement (IHI), published work by the NYC Health + Hospitals (“Embedding Equity into Every Step of Adverse Event Analysis”) that thoughtfully analyzed opportunities to advance equity in health care. Acknowledging the limits of standard root cause analysis (RCA) methods and other patient safety investigation tool(s) to identify the influence of bias and inequity, NYC Health + Hospitals’ description of their approach provided something of a roadmap for our team to follow.
The involvement of WellSpan Health (York, Pennsylvania, USA) in the IHI Leadership Alliance, participation in IHI’s Pursuing Equity initiative, and membership in the Rise to Health Coalition are some indications of our health system leadership’s strong commitment to addressing health inequities in our communities. Before we saw NYC Health + Hospital’s work, WellSpan had been reviewing and analyzing our serious event data for equity, although the work was rudimentary. Intrigued by the NYC Health + Hospitals’ efforts and beginning with the challenges inherent in event analysis, WellSpan performed an introspective analysis using a crosswalk of those challenge “categories” for improvement opportunities.
We reviewed event reporting, investigation, and root cause analysis categories and related principles and conducted a self-assessment. We classified our efforts as “Met,” “Partially Met,” or “Not Met” and assigned a numerical identifier. (See Figure 1 below.)
Figure 1. WellSpan Event Reporting
Categories-Principles | Self-Assessment Status |
WellSpan Event Reporting | |
| Knowledge & comfort: Training and standard tool for identification of bias with everyday examples of bias in patient safety events. | 1 - Partially met – We highlight equity and recognition of bias in new employee orientation for event reporting. We could do more to provide examples of how bias may impact safety event reporting. |
| Data methodology: Embed mandatory fields for demographic and social determinants. Information into the event reporting system and embed a mandatory question into the event reporting system: “Did bias or equitable care issues potentially contribute to this event?” | 2 - Partially met – We have demographic fields available in S1 (patient safety reporting system) and use that to abstract/trend. The barrier is the current patient safety reporting system limitations. We are evaluating this. Further, as highlighted in the IHI Improving Health Equity: Assessment Tool for Health Care Organizations, we could benefit from additional training and education programs that foster a deeper understanding of how to communicate about bias and equity issues, “have the conversation,” and keep communication open and positive. The Patient Safety Team has been engaged in education in expanded Just Culture, Psychological First Aid, Humble Inquiry, Human Factors, etc. |
| Leadership support: Leaders encourage staff to report events and build psychological safety and recognition for reporting. | Met - WSH Leaders have fostered the Just Culture principles of psychological safety to encourage increased safety event reporting. In CY21-CY22, safety event reporting doubled, from just over 20,000 to more than 40,000 reports (a 97% increase), while at the same time decreasing serious events by 45%. |
Investigation | |
| Knowledge & comfort: Training for investigators on identification of bias and equitable care issues, including how to interview staff with a focus on equity. | 3 - Partially met – We have initiated training (humble inquiry) and discussed importance of equity being a part of the investigation. We could simulate these interactions in the future, and model how to best collect this data. |
| Data methodology: Ensure we build equity data fields into the electronic medical record for easy identification for the RCA write-up. | Met – The electronic health record includes equity data fields including but not limited to Race, Age, Gender, Ethnicity, Language preference and Interpreter needs, Payer, Military Veteran status, Vision, Hearing or other physical disabilities/needs and Sexual Orientation Gender Identity (SOGI). |
| Leadership support: Risk management and patient safety leadership set expectations to include an equity lens in the investigation process. | Met - All Serious Event Notification Calls (SENC) begin with the demographic description of how the patient identifies and reports, including Race, Age, Gender, Ethnicity, Language and Payer groups. We consider this information in the comprehensive investigation of root cause to determine if bias may have contributed to any event, or if there is any identified disparity compared to other groups. |
Root Cause Analysis | |
| Knowledge & comfort: Use standard tools for identification of bias and equitable care issues discussed during the RCAs. Share evidence of existing equitable care issues for the adverse event either in literature or past data. | 4 - Partially met – We could do more to standardize tools system-wide. These guidelines will assist in revision/enhancement of our current RCA process. |
| Data methodology: Integrate social determinants of health data into the RCA standard form. Incorporate a bias section into fishbone diagram. | 5 - Partially met – Equity is part of the conversation on SENCs. We could do more to ensure it is part of review output and data collection from RCAs. Expanding demographic information to include insecurities identified by the social determinants of health questionnaire would add value. Complexities include the integration of intervention and follow up for those identified needs. |
| Leadership support: Executive leadership ensures time is set aside in the RCA for an equity discussion and helps facilitate the discussion. Incorporate equity discussion of adverse events in dialogue with the highest levels of leadership. | 6 - Partially met – We have begun to include equity as part of the patient safety conversation, including self-assessing for opportunities where bias may be a contributor to a safety event. These conversations are often uncomfortable but improve with support and continued incorporation into how we do our work. |
Corrective Action Planning | |
| Knowledge & comfort: Provide training on types of interventions that reduce inequities. | 7 - Partially met – There is (voluntary) training available regarding microaggressions, having a conversation about bias (including tools to help to mitigate/improve), and diversity and inclusion. A standard procedure for what, when, and how to implement/spread is currently absent. |
| Data methodology: Investigate historical data on inequities with other similar adverse events. Set an aim statement to reduce bias/focus on equitable care issues in the current event and track data over time. | 8 - Partially met – We have investigated historical data for disparities and are applying statistical analysis for equity. We are just beginning a manual approach to identify bias wording in the written narrative of the safety event. We have also discussed this at our Health Equity Subcommittee for comments, thoughts, and next steps. |
| Leadership support: Regularly report on corrective action progress with an equity lens in departmental and hospital-wide meetings. | 9 - Partially met – Patient Safety Committees regularly report on action plan progress, but not with an “equity lens.” There is reporting on safety trends to our Regional Boards and the Quality Committee, and we also analyze these trends for race, age, gender, ethnicity, and language equity. |
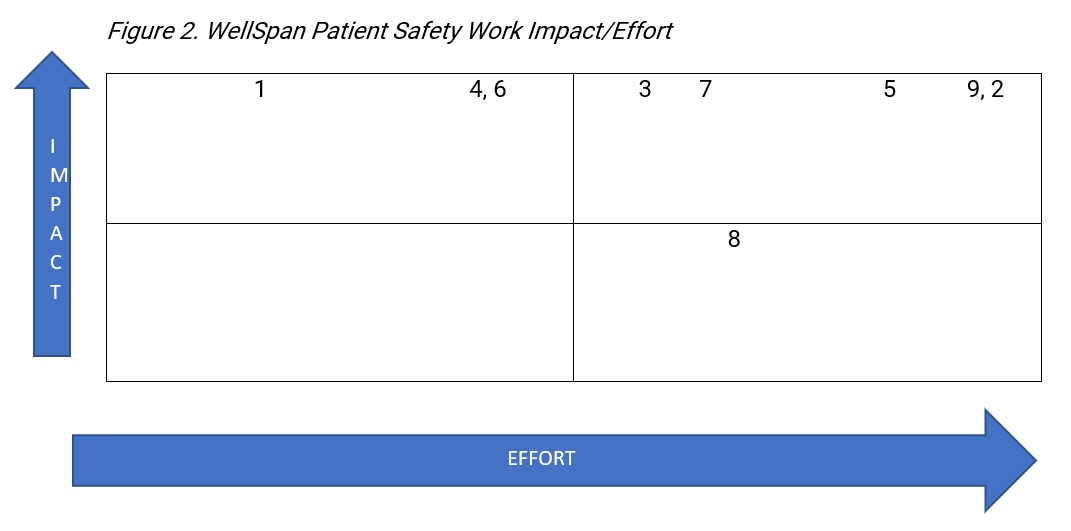
After we completed our self-assessment, we designed a four-quadrant scatterplot tool to help us easily visualize the challenges for overall perceived impact to patient safety and the related work effort or “lift” of each opportunity (see Figure 2 below). WellSpan has prioritized event analysis for equity and performed a related self-analysis for gaps and opportunities based on the related challenge categories and principles outlined by NYC Health + Hospitals. Acknowledging the important value of every safety event principle, this assessment and related four-quadrant plotting for impact and effort highlights the “high impact, low effort” (“low hanging fruit”) and all other opportunities for informed planning of short- and long-term interventions.
Continuing in the “all teach, all learn” spirit demonstrated by NYC Health + Hospitals, WellSpan is sharing our analysis so others might likewise learn from our efforts. This exercise helped us focus on equity in serious event analysis and provided clear initial steps to close the gaps we identified. Any hospital or health system similarly interested in improvement will likely get different results, but we hope they learn as we did from what they find.
Michael B. Seim, MD, is WellSpan Health’s Senior Vice President and Chief Quality Officer. Jodi R. Cichetti, RN, MS, CCM, CPHQ, HACP, is WellSpan Health's Vice President Quality and Patient Safety. Travis Mitchell, MSHA, CPPS, CPHQ, is WellSpan Health's Senior Director Patient Safety.