Why It Matters
When addressing joy in work and well-being, teams can anticipate and address common challenges, including how to engage a leader who is not yet your biggest champion.
“In the early days, you could actually see people cringe.”
Institute for Healthcare Improvement (IHI) Former President and Chief Executive and IHI Senior Fellow Derek Feeley recalled this response when he and others began teaching about joy in work nearly a decade ago. While some in health care embraced discussion of their well-being with relief, others were not so sure.
Feeley approached those who expressed doubt with curiosity. “I would ask people,” he recounted, “’Why is joy in work such a difficult concept for you?’” Most often, he found people demoralized by the dissatisfaction and burnout they witnessed and experienced. They had difficulty imagining how things could ever change. “People couldn't see a path to get from how they were feeling in that moment to anything that they could possibly describe as joy,” said Feeley.
The experiences of health care workers from around the world helped spur the creation of the IHI Framework for Improving Joy in Work. IHI’s goal was to offer what Feeley called in a recent interview “a navigational beacon to help people get from a sense of hopelessness and helplessness to feeling a sense of achievement, meaning, and purpose.”
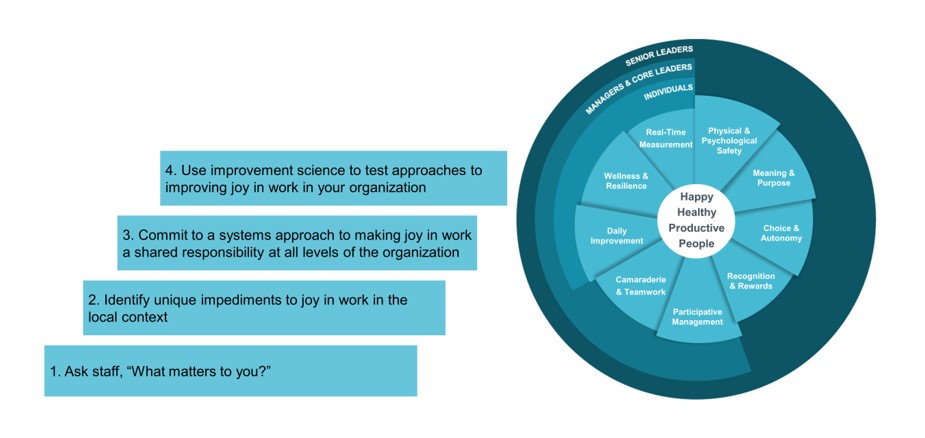
Figure 1. IHI Framework for Improving Joy in Work
In the following interview, Feeley — who is faculty for IHI’s Creating Workforce Joy and Well-Being online course — reflects on the COVID-19 pandemic’s impact on joy in work and well-being in health care and his advice for anticipating and addressing the most common joy in work challenges.
On burnout and COVID
I think focusing on joy in work and well-being has never been so important. IHI chose to work on this before [the pandemic] because it was clear we could no longer ignore burnout. A National Academy of Medicine report (Taking Action Clinician Burnout) came out in 2019 and suggested that somewhere between 35 and 50 percent of US doctors and nurses had symptoms of burnout. And then COVID hit us and things got much, much worse. I think we’re getting a developing understanding of what the pandemic has meant for burnout and for joy in work, which I would argue is its antidote. But it’s an incomplete picture. I’m wondering, for example, if burnout may be another strand of long COVID.
On a notable recent study
There was a massive study done in Australia ("Burn-out in the health workforce during the COVID-19 pandemic: opportunities for workplace and leadership approaches to improve well-being") by Natasha Smallwood and her colleagues. I believe it’s the largest national survey of the health care workforce ever done anywhere in the world. There were nearly 10,000 respondents. Over 70 percent of respondents reported experiencing moderate to severe symptoms of emotional exhaustion. They also found that 40 percent of the workforce reported PTSD symptoms. It was particularly disturbing that 1 in 10 Australian health care workers reported occasional or frequent thoughts of suicide or self-harm during the pandemic. People’s lives are at stake if we ignore that.
Online Course with Coaching: Creating Workforce Joy and Well-Being
On how proximity to patients and equity influence staff experience
The Australian study also indicated that the greater your proximity to patients, the higher your likelihood of experiencing symptoms of burnout. Junior staff are also more likely to experience these symptoms. Also, NHS research has shown that staff of color in health care are more likely to be in disciplinary procedures, more likely to be subject to bullying and harassment, and more likely to feel that it’s not safe to speak up about problems. This is true in the UK, and I’ve seen no evidence that this would be different in the US. It’s hardly any wonder that staff of color feel more significantly impacted by burnout.
On the inverse relationship between joy in work and burnout
in the second phase of our joy in work efforts in with Safer Care Victoria in Australia in Victoria, we can now show that as joy in work increases, burnout scores go down. It increases our degree of belief in the theory. I’ve seen it implemented now across the world. To paraphrase the statistician George Box, “All frameworks are flawed, some are useful.” This is definitely a useful framework.
On common joy in work challenges and how to address them
Addressing these challenges requires a proactive and flexible approach:
Don't let measurement get in the way of getting started on joy in work and well-being. The most common challenge people face when implementing joy in work and well-being efforts is around measurement, especially getting frequent enough measures to gauge improvement in a world where we typically rely on annual surveys. Leaders should accept that measurement may not be perfect and focus on gathering enough intelligence to assess whether things are moving in the right direction. Whether it's a pebble in a jar or a thumbs up or a thumbs down to indicate if it was a good or bad day when people leave for the day, just accept that the data you will collect will be imperfect, but it'll probably give you enough to make some kind of assessment about whether things are moving in the right direction or not. And let the measurement flow from your activities rather than letting your activities be governed by what you can measure.
Always remember that context matters. Joy in work is highly contextually sensitive, and interventions that worked in one setting may need adaptation for local context. This is what makes scale up and spread quite challenging. Leaders should be aware of this and be ready to make necessary adjustments.
Executive sponsorship is essential. Leadership support is important for removing barriers and facilitating progress. I see teams with active executive sponsors make progress more quickly and engage with leaders throughout an organization more effectively than those who struggle to engage their leaders.
On what teams can say to leaders they are struggling to engage
I often preface any presentation I'm giving about joy in work by saying, “I think this is the most important thing for leaders in health care to focus on right now. I can’t think of anything more important than taking care of our caregivers.” When we invest in joy in work, we are also investing in patient safety because we can point to connections between staff who feel engaged and looked after and improvements in patient safety. We can show how by working on joy in work, you can reduce turnover in your workforce. So, there's a business case for working on joy. I know joy in work and staff engagement are not the same, but I think it’s reasonable to suggest that they're connected. And when Gallup compared employee engagement, they found a 58 percent difference between top- and bottom-quartile organizations when they looked at patient safety incidents. What other way can we reduce patient safety problems so dramatically? If a health care leader asked me what one thing could be done to improve patient safety, I’d say, “Demonstrate to your staff that you genuinely care about them.”
Editor’s note: If you or someone you know is struggling or in crisis, help is available. In the US, please call or text 988 or visit 988lifeline.org. In the UK, call 116 123 to talk to Samaritans, or email jo@samaritans.org for a reply within 24 hours.
Additional editor’s note: This interview has been edited for length and clarity.
