Why It Matters
Quality should be everyone’s job in a health care organization. Yet, as the Juran Handbook points out, supporting quality also requires a dedicated team.
Aligning with whole system quality — a more holistic approach to quality management — requires deep investment in quality control systems (such as tiered, escalating huddles and role-based standard work), quality planning (using feedback from patients, community members, employees, and other key customers to set strategy), and quality improvement (applying the science of improvement to achieve the resulting aims and close performance gaps).
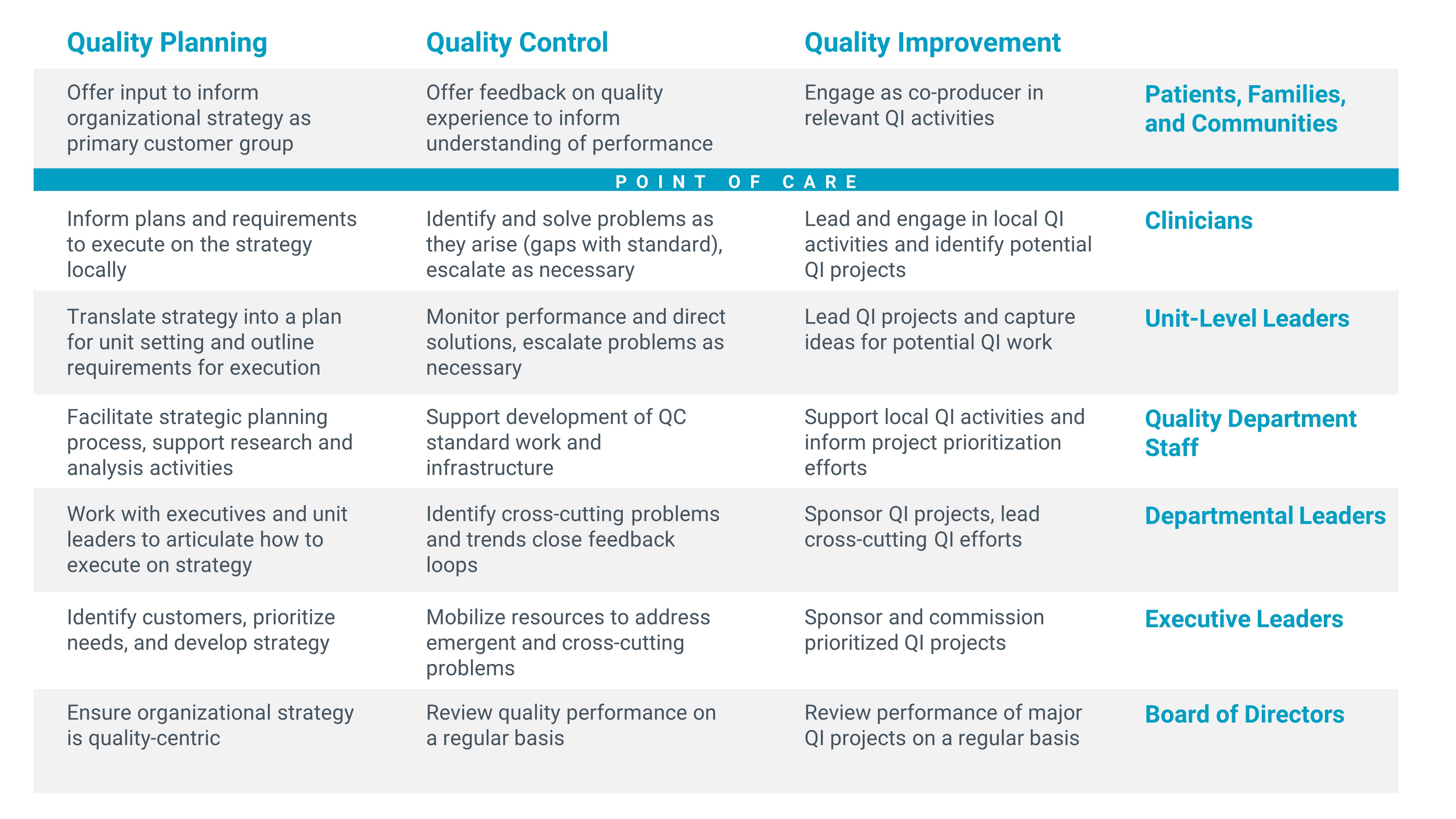
Whole System Quality Approach: Quality Planning, Quality Control, and Quality Improvement Activities by Stakeholder Group (Source: Whole System Quality: A Unified Approach to Building Responsive, Resilient Health Care Systems IHI White Paper)
Yet, health care systems have few sources of guidance regarding how to structure their quality teams and the roles those employed in quality should play.
The Quality Department’s Typical Role
Quality managers often focus heavily on quality assurance and compliance. They collect data to satisfy the requirements of regulators, accreditors, and others who monitor health system performance (e.g., US News or Leapfrog); identify gaps between current and target performance; and work with clinicians to close those gaps. Also, quality managers often play a key role in quality improvement training and in supporting safety and infection control efforts throughout the organization.
As demands on them increase, quality managers report being stretched thin and having inadequate resources to do the many tasks required. In addition to traditional quality work, their responsibilities often now include population health management or managing patient experience efforts.
The Challenge of Organizational Structure
In addition to challenges with clear role definition, hospitals and health care systems often struggle to identify the best organizational structure for their quality teams. The Institute for Healthcare Improvement (IHI) innovation team used its 90-Day Learning Cycle to investigate the role and structure of health care system quality assets and found that no single design will promote improved outcomes and efficient resource use. For example, a McKinsey study found that the configuration selected for quality (e.g., less or more centralized) matters less than how it is achieved.
While the broader literature offers support for certain keys to organizing successful quality departments — such as reporting to a member of the executive team and ensuring adequate resources — research on quality organizational structures still includes many gaps and conflicting findings.
At the same time, certain considerations did emerge from the research that can help health care systems structure quality teams:
- Bring the right people together. If disparate quality roles report to different leaders, organizations can build more cohesive structures. For example, the newly appointed quality director of one hospital we investigated brought functions such as infection control, performance improvement, and quality data analytics together under one reporting structure because she believed it was essential to make an impact on quality. Building a clear vision and set of values for this new team also helped build a foundation for a more targeted and coherent quality approach.
- Bridge gaps between disparate quality functions and facilities. For example, one system initiated corporate roles over safety, performance improvement, and reporting. While site-level staff report to site-level quality directors, these corporate director roles promote consistency across sites and enable shared learning.
- Consider clearer distinctions between quality assurance, quality improvement, and quality planning. For example, one system has significant investment of specialized staff focused on assurance while different staff focus on improvement. This distinction helps ensure that the organization does not disproportionately dedicate quality resources to compliance activities over coaching for improvement.
Innovations in Quality Roles
Two organizations have identified innovative ways for patients to play crucial roles in quality:
- At East London NHS Foundation Trust (ELFT), patients (known as service users) play a formal role in the quality system – within the planning process, the improvement work, and the assurance program. ELFT invited service users to design a new accreditation program to define the standards they would expect for excellent quality care. More than 60 ELFT service users are now trained as assessors who visit services to evaluate how the care aligns with these standards. The service user-led accreditation program awards services with gold, silver, or bronze levels of accreditation; identifies opportunities for improvement for every service; and works with the service to make these improvements. The program makes quality assurance a more meaningful activity for both patients and staff, and its structure helps promote equity because the service user assessors are representative of the overall patient population and can point to equity risks.
- At Southcentral Foundation in Alaska, the quality planning process begins with the patient (“customer-owner”). The voice of the customer sets the priorities for work and services provided at Southcentral Foundation. The articulation of what matters to patients as a set of principles informs all quality improvement work throughout the year, reinforced by all members of the organization and supported by the quality team. When teams identify potential improvement projects, they are checked against priorities and supported by quality specialists.
To advance a whole system approach to quality, the quality team plays a key role in supporting the systems necessary to advance quality planning, control, and improvement. Quality is everybody’s job, but quality specialists offer invaluable training, resources, strategic guidance, and support with prioritization. They help to advance the quality of the quality management system itself. Quality managers can advance new ways to staff quality activities with the right balance between quality planning, improvement, control, and assurance and can also ensure that quality activities put patients first.
Jeffrey Rakover, MPP, is an IHI Director, Innovation. He thanks Amar Shah, Chief Quality Officer, East London NHS Foundation Trust, and Michelle Aregood, Director of Quality Assurance, Southcentral Foundation, for their contributions to this story.
You may also be interested in:
IHI Whole System Quality white paper
IHI Sustaining Improvement white paper
