Why It Matters

Photo by Bonnie Kittle | Unsplash
As improvers and leaders of improvement, many of us are very familiar with the three questions of the Model for Improvement, developed by Associates in Process Improvement:
- What are we trying to accomplish?
- How will we know that a change is an improvement?
- What change can we make that will result in improvement?
As an improvement advisor, when I ask teams what word across these three questions is most critical for improvement and long-term sustainability, I often get these answers:
Accomplish
Change
Improvement
To be sure, these are all important elements. However, as Kate Hilton has noted when talking about the Psychology of Change, none of these are at the root of what most matters for sustained improvement in a system. It is a small, easy-to-gloss-over word common to all three questions. Do you see it?
- What are WE trying to accomplish?
- How will WE know that a change is an improvement?
- What change can WE make that will result in improvement?
Because it is almost impossible for one person to make lasting and meaningful change within a system on their own, we must establish trust within our improvement teams. In fact, I would argue that quality improvement happens at the speed of trust. An aim might be clear and motivating, the changes may be designed for impact, and the data may be full of insights, but a lack of trust can undermine all our efforts. We take a big risk when we ignore this element of improvement or mistakenly assume trust is there.
More broadly, to improve outcomes, reduce inequities, and strengthen workforce well-being, organizational trustworthiness matters for health care systems. Working toward any of these aims without addressing trust misses a crucial element of improvement.
Earning trust may be more important than ever for health care. The percentage of the public saying they had a “great deal” or “quite a lot” of confidence in the medical system dropped from 80 percent in 1975 to 37 percent in 2015. While all American institutions have seen declines in trust over this period, the drop has been greatest in the health sector. Medical mistrust is even deeper in communities of color. An October 2020 poll by ESPN’s The Undefeated and the Kaiser Family Foundation found that 7 in 10 African Americans believe that people are treated unfairly based on race or ethnicity when they seek medical care.
With support from the American Board of Internal Medicine Foundation (ABIMF), IHI’s Innovation Team researched drivers of trust between a health system and clinicians and communities. Interviewing nearly 50 interviewees across seven health systems, the Innovation Team found three core reasons behind a lack of trust across both communities and clinicians:
- Misgivings from personal and/or historical experience
- Misdoubts about motivation and/or decision-making
- Misalignment in values
Based on this understanding of what has led to mistrust, the Innovation Team developed a framework for rebuilding and strengthening trust by adapting and building upon a framework known as the Healing ARC developed by Michelle Morse, MD, MPH, and Bram Wispelwey, MD, MPH, of Brigham and Women's Hospital in Boston.
While developing this framework, IHI recognized it was important to do more than explain why trust was broken or simply outline the elements of organizational trustworthiness in health care. The goal was to offer a blueprint for how to build and strengthen trust — intentionally and proactively — where it had been broken or did not previously exist.
In the recently published IHI Innovation Report on Organizational Trustworthiness in Health Care, each step in the framework includes specific actions and change ideas that leaders in health care systems can begin to test to improve trust with clinicians in their system and communities they serve.
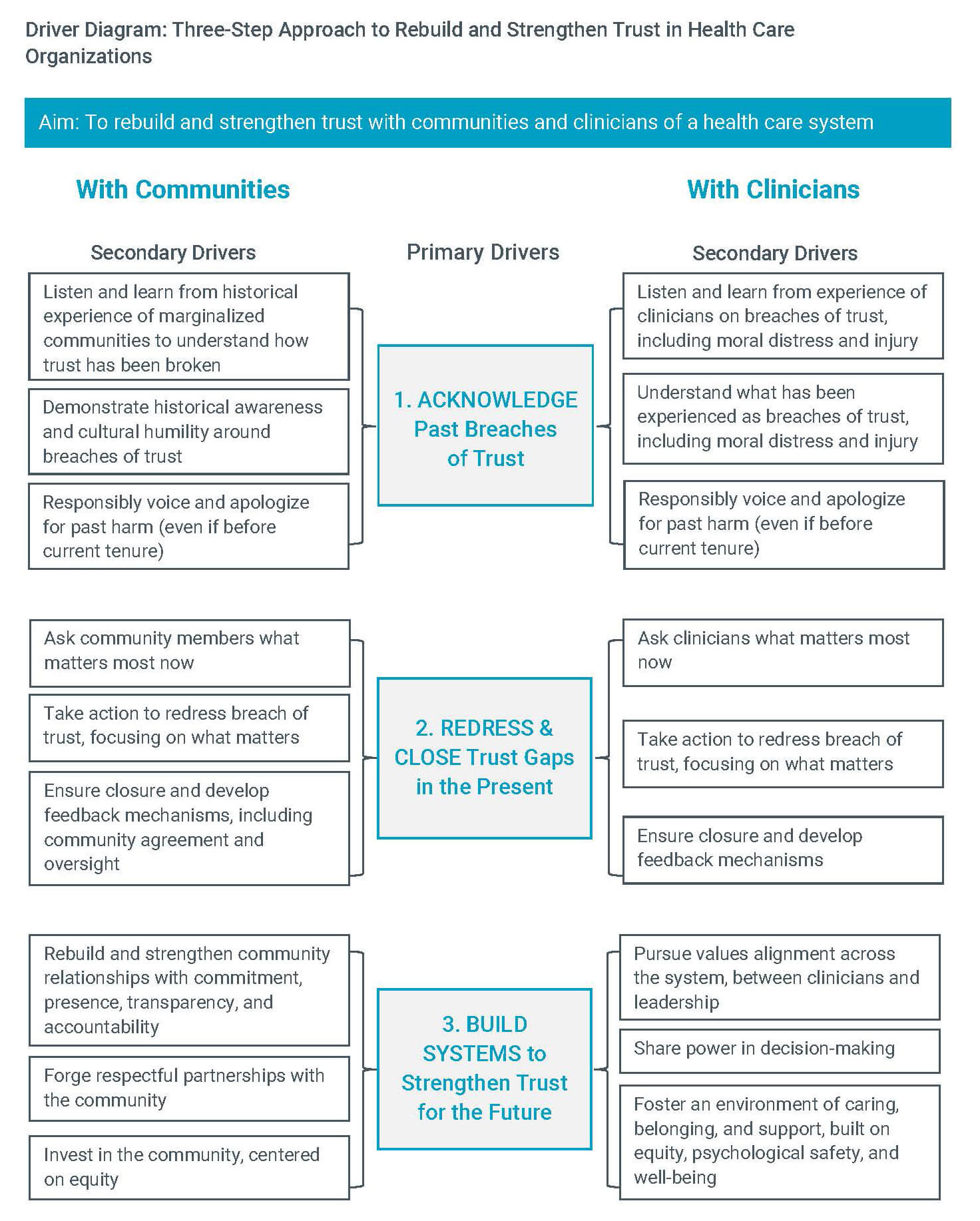
Driver Diagram: Three-Step Approach to Rebuild and Strengthen Trust in Health Care Organizations. Source: Organizational Trustworthiness in Health Care.
Over the next year, IHI and the ABIMF will be supporting health care organizations to build trust with their clinicians and communities to help meet their larger goals of improving patient outcomes, reducing inequities, and strengthening workforce well-being. There is an opportunity is to see a ripple effect not only in this specific work, but across all quality improvement initiatives for all who take part in this prototyping community.
Tricia Bolender, MBA, MA, is faculty and an improvement advisor for the Institute for Healthcare Improvement.
You may also be interested in:
Science Direct — A matter of trust: Commitment to act for health equity
It’s Not You, It’s Us: Earning Trust to Build Community Connections
