Why It Matters
The Institute for Healthcare Improvement (IHI) partnered with the Australian quality and safety agency, Safer Care Victoria (SCV), to improve birthing outcomes for women and babies. Between March 2019 and July 2021 (with a six-month pause in 2020 due to the COVID-19 pandemic), 35 teams from maternity services across the state of Victoria participated in two large-scale quality improvement programs:
- The Better Births for Women Collaborative aimed to reduce harm to Victorian women by preventing severe third- and fourth-degree perineal tears. It achieved a 45 percent reduction in severe perineal tears, from an average rate of 4.41 percent to 2.44 percent across participating teams, which equated to approximately 155 women avoiding this harm (see Figure 1).
- The Safer Baby Collaborative aimed to reduce the rate of avoidable stillbirths in the third trimester of pregnancy. At the collaborative’s completion, there was a 113 percent increase in the average days between stillbirths from 3.5 to 8.1 days, indicating that stillbirths in the third trimester were occurring less frequently at participating health services (see Figure 2).
Various factors contributed to the success of these collaboratives, but one deemed important to those that participated was the priority placed on supporting teams to use data and narrative to tell compelling stories about why these projects mattered, what impact the work was having, and what more could be done to improve outcomes. The collaboratives utilised their measurement strategies — alongside consumer and clinician experiences — to make the case for improvement and guide collective efforts towards the aims. This powerful combination of quantitative and qualitative data informed and engaged participating teams across the state to deliver significant improvements.
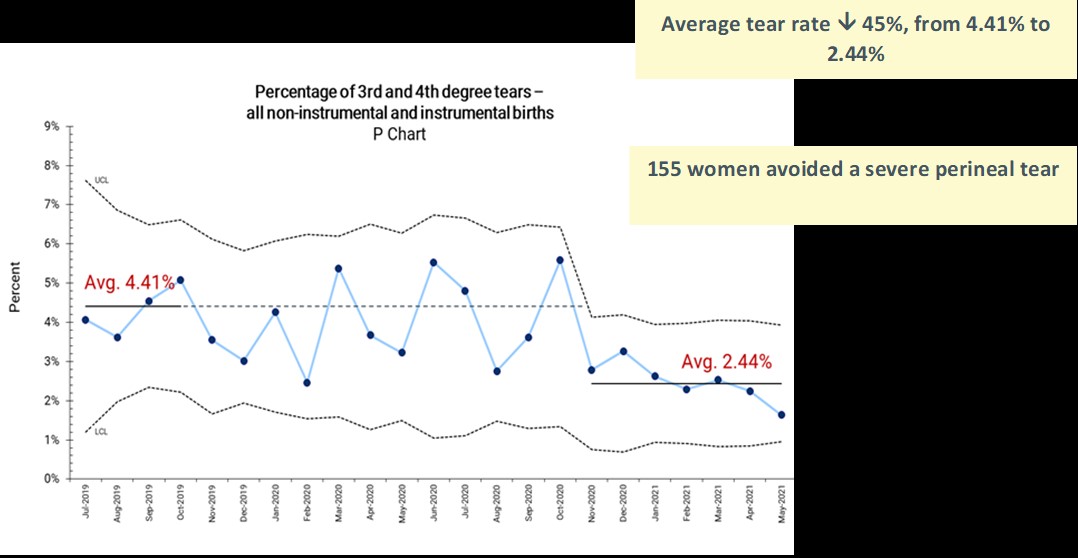
Figure 1. Percentage of 3rd and 4th degree perineal tears
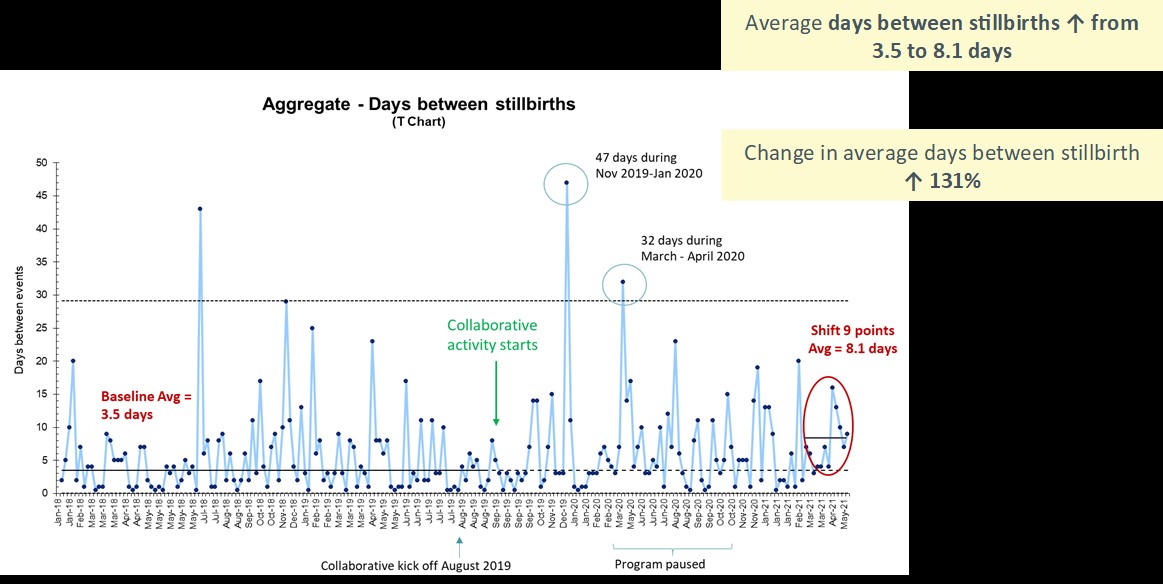
Figure 2. Number of days between stillbirths
Going Beyond Numbers
When the Safer Baby Collaborative was launched, participating teams were advised that Victoria’s stillbirth rate was 6.2 per 1,000 births after 20 weeks, and 2.2 per 1,000 births at 28 weeks or more. These statistics failed to adequately communicate the devastation associated with stillbirth. As Paul Brodeur, an American investigative science writer and author once stated, “statistics are human beings with the tears wiped off.” This sentiment rang true in this collaborative as parents shared heart-breaking accounts about their experience of losing a baby and the ripple effects felt by other siblings, uncles, aunts, cousins, grandparents, and friends. These stories, along with clinicians’ stories of caring for families when their babies died, brought to light the real impact and grief associated with each stillbirth counted in the state-wide statistics. Participating teams found these personal accounts deeply motivating, which helped to build will and focus their improvement efforts.
A highly sensitive but crucial part of the narrative for the Better Births for Women Collaborative was the extent of the often hidden harm caused to women by perineal trauma. Hearing directly from women about long-lasting physical and psychological impacts, clinicians shifted their level of acceptance of perineal tearing. A shared understanding emerged of the critical importance of the issue to women’s health and well-being, and a recognition that in many cases this harm was preventable. It was clear from the descriptions of trauma endured by women that severe perineal tears were not something that should be tolerated or normalised. These stories compelled participating teams to partner with women and change clinical practices, embedding processes to reduce potential harm from occurring (e.g., a warm perineal compress, techniques to encourage a slow, controlled birth, and an episiotomy when clinically indicated).
Measurement Informed by Lived Experience
Collaborative measurement strategies were developed with expert panels which included consumers with lived experience of perineal tears or stillbirth, midwives, obstetricians, maternity service leaders, and improvement experts. Consumers informed the selection of measures to ensure they addressed what matters most across all stages of pregnancy and birth, particularly to encourage women to participate actively throughout their maternity care, and be well informed when making decisions.
Clinicians also contributed to measurement selection and validated alignment with best practice. They ensured measures were appropriate and practical in a wide range of settings, including maternity services delivering anywhere between 200 to 7,000 babies a year. Clinicians helped refine the final combination of measures so they captured data on key outcomes and critical process steps. They also identified unintended consequences that may occur as a result of the collaboratives so these could be identified and appropriately addressed. Utilising input from the expert panel of consumers, clinicians, and improvement practitioners meant only essential data to inform improvement efforts were selected and that data collection was not overly burdensome.
Changing the Narrative to Drive Local Improvements
Teams collected data for their own maternity services, plus engaged consumers throughout every stage of design, delivery, and evaluation of the two collaboratives. In the early phases, many teams held the view that they were already delivering care aligning with best practice. However, their baseline data, coupled with powerful stories from women who had received maternity care at their health service, highlighted opportunities to improve the reliability of providing components of care deemed important to reduce perineal tears or the risk of stillbirth. This offered a compelling case for participating in the collaboratives and motivated teams to test change ideas to more consistently deliver evidence-based care.
By monitoring measures and gathering feedback while testing change ideas using rapid Plan-Do-Study-Act (PDSA) cycles, teams could identify what changes were or were not working within their service. They used this data to inform their team-level improvement narratives and systematically refined change ideas until they were having a positive impact. Teams shared this learning and narrative with other participating maternity services to accelerate the pace of improvement across the state. Not only did this data help support the compelling reasons for change, but it enabled frontline teams to know they had the power and ideas to make improvements happen.
Applying the Art of Storytelling: Beginning, Middle, End
“In the beginning . . . there was unclear or differing advice being provided to women.”
“In the beginning . . . we realised we needed to act NOW!”
The art of storytelling was used by consumers, clinicians, and participating teams throughout the collaboratives. Learning sessions were used to discuss effective approaches to telling stories and communicating key messages. Much like every good Disney story, teams were encouraged to include a clear beginning, middle and end. This structure enabled them to succinctly share their learning around how their maternity service was performing, what they were achieving, how they did it, and what this meant for women and babies. The stories provided rich insights into their improvement journeys about the successes, “fail forwards,” and unexpected bumps along the way. Teams humanised their measures by getting consumers and clinicians to describe the real impact on them as individuals. Interweaving various sources of data within these stories fostered commitment, collaboration, and ultimately achievement.
“In the middle . . . we were struggling to challenge norms around decreased fetal movement management.”
“In the middle . . . despite the pandemic, we decided we couldn’t just stop. The work was too important.”
A key lesson learned in these projects was that facts don’t get in the way of a good story; they are a crucial part of the story. A measurement strategy that addresses what matters to consumers and clinicians — combined with personal narratives from those with a lived experience — creates a compelling story that inspires and supports teams to sustain impactful results.
“But it’s not the end . . . We will keep on going, shamelessly stealing, sharing tips, tricks, and ideas!”
“But it’s not the end . . . We won’t stop working on improvement.”
Lisa McKenzie is Regional Director, Asia Pacific, for the Institute for Healthcare Improvement. Rebecca Reed is an Improvement Advisor for Safer Care Victoria. Felicity Czarnecki is Collaborative Director for Safer Care Victoria.
