Why It Matters
Photo by Pontus Wellgraf | Unsplash
When the team from the Oregon Health & Science University (OHSU) first decided to examine the equity of their care for older adults, they faced some challenges. For one thing, it was the early days of the COVID-19 pandemic. Identifying and engaging stakeholders amid so much uncertainty and new demands was not easy.
“Nobody wanted to hear about a new quality improvement measure,” recalled Emily Morgan, MD, a physician specializing in geriatric medicine at OHSU. “Some people were interested in hearing about something other than about COVID, so that was kind of on my side, but people were exhausted. They felt like their providers were already experiencing burnout because they were not meeting metrics.”
Like participants in other health care quality improvement initiatives, Age-Friendly Health Systems (AFHS) organizations had to adapt to the realities of the pandemic while staying focused on providing optimal care for older adults. To encourage engagement in their AFHS equity work, OHSU focused on learning rather than meeting targets. Instead of setting arbitrary metrics, the ask was to “see how we’re doing, and then let’s try to get better,” Morgan explained. “There was no baseline to meet. We didn’t want to demoralize staff by telling them they weren’t doing something well.”
The resulting study published about the age-friendly work at OHSU is the first to include data about health equity as part of AFHS outcomes and illustrates the importance of creating equitable care at clinical and institutional policy levels.
Assessing Equity
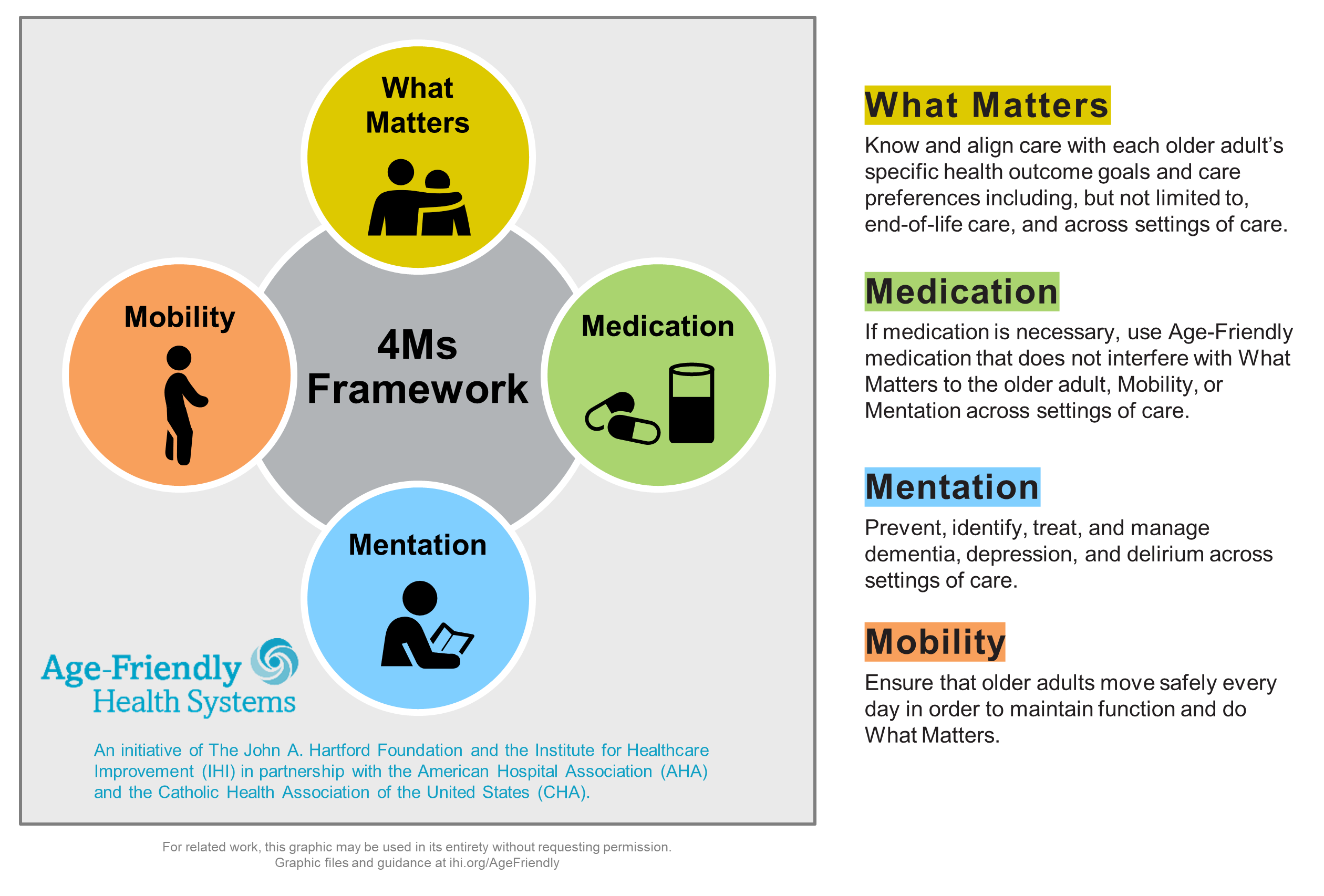
AFHS is an initiative of The John A. Hartford Foundation and the Institute for Healthcare Improvement (IHI) in partnership with the American Hospital Association (AHA) and the Catholic Health Association of the United States (CHA). Its goal is to follow evidence-based practices while minimizing harm in older patients. The evidence-based elements of high-quality care are known as the 4Ms: What Matters, Medication, Mentation, and Mobility.
The five metrics OHSU used to measure health equity were gender, race, ethnicity, preferred language, and electronic patient portal activation. OHSU’s data showed that between April 2020 and April 2021, 3,370 patients had at least one clinic visit. Of those, 56.9 percent identified as female, and 43.1 percent identified as male. Most patients were White (86.2 percent), non-Hispanic (90.8 percent), and indicated English as their primary language (96.8 percent).
When broken down into the essential elements of the 4Ms, 57.3 percent of patients had undergone cognitive screening, 57.2 percent completed a depression screening, 47.6 percent had advance care planning, and 40.6 percent had a mobility assessment. Overall, only 15.3 percent of patients received care that included all 4Ms.
Patients with active electronic patient portal accounts were more likely to have been prescribed high-risk medications than those who did not. In addition, high-risk medications such as benzodiazepines, tricyclic antidepressants, and paroxetine tended to be prescribed to women than men. Patients were 73 years old on average and were predominately non-Hispanic White (86.9 percent), English-speaking (98 percent), and female (61.7 percent).
The root cause for these differences is yet to be determined, but theories include whether a patient has a caregiver or proxy who is helping them by being active on the patient portal on their behalf or how inclined patients are to advocate for themselves and raise concerns about experiencing side effects. Their efforts found that most older adults are open to deprescribing if recommended by their primary care physician.
Of the 4Ms, the What Matters metric had the most statistically significant pairings. Conversations about advance care planning occurred more often with females than males and with English speakers more than non-English speakers.
The region served by OHSU is predominantly White and English-speaking. The lack of diversity in the patient population reflected the demographics of the area, but the OHSU team acknowledged that when studied in a broader scale, patterns in the data may shift, and can be scaled to address the gaps in other settings. They recommended future studies to identify gaps in AFHS care in regions with more diverse demographics, and to provide more insight into the root causes of these disparities.
Gaining Momentum
Initially, gathering every stakeholder across 12 clinics was difficult, particularly with COVID in play. Each clinic had its own focus and people with different health care delivery priorities and getting them all to agree that the health equity data that came out of their age-friendly initiative was a huge win.
The OHSU team was fortunate that there has been system-wide interest in closing equity gaps. “I’ve been at OHSU for 11 years, and I’ve seen pockets over the years and little groups really invested in What Matters care. I have never seen a groundswell like this,” said Katie Drago, MD, an assistant professor of medicine at the Division of General Internal Medicine and Geriatrics. “We have general internal medicine champions from this clinic that are leading the charge to create one sort of throughput, one story about goal-concordant care values, desires, and wishes that may start either in the inpatient or ambulatory sphere depending on where the patient enters into our health system.” This information is readily available to providers across settings that use their EHR, including in other clinics, specialty practices, inpatient care, intensive care, or long-term care. “This process of integrating what we discovered in the data is going to be a major overhaul,” Drago explained. “We’re just amassing stakeholders right now, but it’s really involving everybody.” So far, goal concordant care has been identified as an institutional quality priority as well as aligning high-risk medication reduction with quality metrics for risk payment models in ambulatory care.
Making Data Collection Easy
At the beginning, the team working on health equity used a simple electronic spreadsheet to collect their AFHS data. With the help of one of their MPH students, over time they began using data visualization software. But Drago suggested that a team could collect health equity data in any document if they were starting with one unit or team. “It may be a little labor intensive, but you’ve got to start somewhere,” she said.
For OHSU, making the data easy for all the clinics to work with was an essential part of the process. “I set it up so that it automatically gets pulled and turned into these beautiful charts and graphs and is university-wide, clinic specific, and gets sent out every month,” Morgan explained. Making data collection difficult, she said, would essentially stop it from happening, especially in a large system. “Each clinic has to do it in a very digestible way,” she added.
According to Drago, approximately 14,000 older adults have been touched by the 4Ms initiative at OHSU between 2020 and 2022. While she does not yet have the data to understand the outcome-based effects of getting all 4Ms, she found what the data said about their reach surprising. “I was floored, truly floored [by the numbers]. And these are people who received all 4Ms.” The number includes all OHSU acute care hospitals and 12 primary care clinics.
Drago’s ultimate goal is to ensure that all the older adults that interact with OHSU’s system in any setting receive 4Ms care. “Our performance should be 100 percent across the board,” she said. While acknowledging they still have a way to go, Drago see age-friendly care as pointing them in the right direction. “My North Star is to make sure that every older adult that we touch receives 4Ms care, period,” she asserted.
You may also be interested in:
Age-Friendly Health Systems resources
Using the Age-Friendly 4Ms to Better Advocate for Older Adults (and Geriatric Care)
For a Better Health Care Future, Improve Care for Older Adults
