Why It Matters
Racism. Classism. Sexism. Homophobia. Ageism. These and other forms of discrimination and bias are as much a part of the health care system as the rest of society. Many health care providers are eager to do something about this.
But where do we begin?
Abigail Ortiz, MSW, MPH, has some suggestions. She’s Director of Community Health Programs at the Southern Jamaica Plain Health Center (SJPHC) in Boston, Massachusetts. She is also a member of Institute for Healthcare Improvement (IHI) Equity Advisory Group.
Last summer, she and her team began testing a series of questions clinicians can use to open up dialogue and start building trust with their patients. The initiative started when physicians approached her with a simple but important question about how to end health inequity:
“What do we do in the exam room?”
Essential Preparation
Ortiz reached out to interested volunteers who had taken part in the center’s earlier community organizing efforts, a group that ranged from residents to mid-career medical professionals. They agreed that it was important to face racism head on. “We address race explicitly, but not exclusively,” she explained.
The group understood that their good intentions would only get them so far without adequate preparation, so they joined Ortiz for three 7:30 AM meetings in June to:
- Agree on a shared definition of racism (from David Wellman: “a system of advantage based on race”),
- Discuss their values (“What values guide your work? What do these values look like in action?”) to encourage the clinicians to use their hearts and their heads to guide their work, and
- Review the literature (such as the references included in the IHI Achieving Health Equity white paper).
They found implicit bias resources (like those described by WIHI guest Anurag Gupta, MPhil, JD, Founder and CEO of Be More America) especially helpful. Ortiz noted, however, that it was important to acknowledge that differences in access to power means not all bias is the same. “Bias isn’t bias isn’t bias,” Ortiz asserted. “Everybody’s bias doesn’t have equal weight when it plays out around policies, procedures, and practices.”
Opening Dialogue
One member of the group — a white physician whose patients are all people of color — began opening his clinical encounters with this query:
“Many of my patients experience racism in their health care. Are there any experiences you would like to share with me?”
The question immediately opened up an honest conversation. The physician found it so effective, he has started all his patients’ annual physicals with this query for the past year.
Informed by this success, the team at SJPHC developed a series of questions to ask at the start of their clinical encounters:
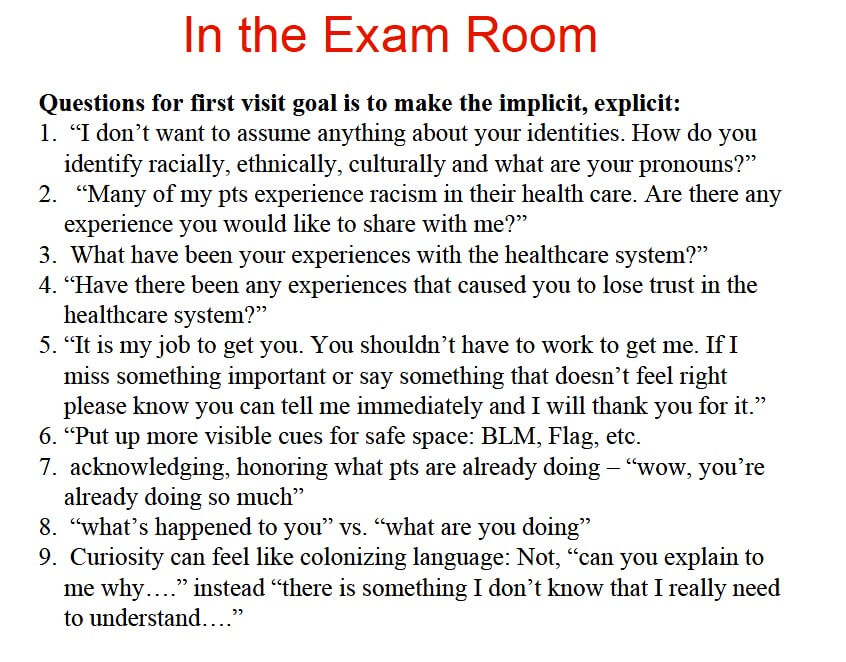
Courtesy of Southern Jamaica Plain Health Center (Boston, Massachusetts)
Similar to the deceptively simple “What matters to you?” query that many clinicians around the world are now using to make their care more person-centered, using these open-ended questions can be powerful ways to open up an important dialogue. The questions are direct, yet respectful. They convey humility in their admission that the doctor does not know all that may be important to understand about a patient. The questions acknowledge that racism isn’t only a product of intentional bias.
The team at SJPHC have been testing these questions throughout the summer. (Ortiz calls them their “Racial Justice PDSAs.”) They hope to have interesting results to share this fall.
